How Scribes Improve Documentation Accuracy by Over 90%
Medical documentation accuracy is not a “nice to have.” It is the difference between a claim that pays versus a denial you fight for 45 minutes. It is the difference between a clean problem list versus a clinical landmine. It is the difference between compliant notes versus audit exposure. The reason scribes move accuracy numbers so fast is simple: they turn documentation into a controlled workflow with checks, structure, and repeatable language. When teams measure accuracy the right way, many see documentation accuracy jump past 90% because the process stops relying on memory, rushed typing, and inconsistent habits.
1) The 90% accuracy jump is not magic. It is measurement + workflow control.
Most organizations say “we want accurate notes,” then measure nothing. Or they measure the wrong thing, like whether the note is long. A scribe driven accuracy system is different. It defines accuracy in auditable components, tracks them, and builds habits around the failure points.
If you want “over 90%,” you need an accuracy scorecard that is strict enough to matter and simple enough to run weekly. Use a rubric with weighted categories:
Correct patient story capture (HPI matches the visit reality)
Required elements present (chief complaint, ROS where needed, exam, assessment, plan)
Coding support and medical necessity wording consistency
Medication, allergy, problem list correctness
Orders, referrals, follow ups and patient instructions clarity
Risk and compliance elements (telehealth specifics, consent, time, attestations)
Provider edits per note and edit type frequency
This is where scribes win. They standardize the “inputs” of documentation. They learn the provider’s clinical style and convert it into consistent note architecture using templates, macros, and structured prompts. That is why training matters. If you are building this as a career path, start with the fundamentals in the complete exam guide and then sharpen your process thinking with the study techniques playbook.
Accuracy is also not only clinical. It is operational. Scheduling context, payer rules, eligibility workflows, and clean handoffs impact what gets documented. If your documentation breaks downstream, you will see it in denials, rework, and provider burnout. That is why tech enabled admin workflows matter too, especially for CM AAs and documentation heavy teams. Pair clinical documentation thinking with the operational mindset in the 2026 documentation trends report and the automation and AI breakdown.
To keep this real, here are the “silent killers” that scribes consistently fix faster than any other role:
Missing medical necessity phrasing that weakens coding support
Templates that look clean but hide inaccurate clinical details
Copy forward that carries old problems into today’s plan
Telehealth notes missing required elements or time documentation
Providers changing the note to match the coding instead of the clinical truth
Medication lists that are “close enough” but wrong
“Follow up PRN” with no timeframe or triggers
If you want your scribe work to translate into future growth, understand the full ladder in the scribe career pathways guide and the employer expectations inside essential skills employers want.
2) The real reason scribes boost accuracy is “cognitive offload” plus structured capture
The provider’s brain is not designed to be a recorder. In a busy clinic, the provider is diagnosing, prioritizing risk, making decisions, and managing the room. Documentation becomes a second job running in parallel. That is where mistakes come from. Scribes remove the split attention problem.
When a scribe is trained properly, accuracy improves because:
They listen for missing specifics and ask for them in real time.
They turn conversation into structured clinical language fast.
They protect against default templates and careless copy forward.
They create a stable note format that coding and compliance can trust.
This is why programs that focus on practical workflow matter. If you want to understand what “good” looks like, compare systems through the lens of exam breakdown expectations and avoid the traps in common exam mistakes.
Accuracy also depends on language. A scribe can make a note longer and still make it wrong. The goal is precision. That is why terminology skill is non negotiable. Build speed and correctness with medical terminology study methods and reinforce through repetition using the interactive practice exam.
Finally, accuracy improves when documentation becomes a feedback loop. Great scribe teams do not “write and forget.” They review denials, provider edits, coder notes, and audit findings. Then they update templates and scripts. This is the same mindset used in admin operations, which is why pairing scribing insight with the CMAA skill set is powerful. See what employers prioritize in top CMAA skills and how certification changes outcomes in career opportunity impact.
3) Where accuracy really breaks: the 8 documentation zones that create 80% of errors
If you want a fast jump in accuracy, stop trying to “be better at documentation.” Target the zones that create repeated failures. Scribes naturally do this because they see the same issues across hundreds of notes.
Zone 1: The patient story is incomplete
If the story lacks timeline, severity, context, and what changed, the assessment becomes guesswork. Scribes fix this by prompting for missing details and capturing them in structured phrasing.
Zone 2: Template behavior overrides reality
Templates help speed. They also hide inaccuracies. Scribes reduce this risk by making “exceptions” visible and ensuring the note reflects today’s specifics.
Zone 3: Telehealth compliance gaps
Remote care amplifies documentation risk. Missing patient location, modality, consent, or time documentation creates compliance exposure. Scribes use checklists and macros to make this automatic. Pair this with understanding remote workflow shifts in remote scribing transformation and the broader admin view in virtual medical administration.
Zone 4: Medication and allergy truth drift
Lists get stale. Patients change meds. A scribe driven med rec prompt at each visit prevents silent chart decay.
Zone 5: Specificity that coding and compliance need
Specificity is not “coding games.” It is clinical clarity. A note that documents laterality, acuity, severity, and rationale is both clinically safer and operationally cleaner. Learn the downstream impacts by reading how documentation supports efficiency in research on scribe impact and revenue outcomes in scribe impact on hospital revenue.
Zone 6: Provider edits become the hidden accuracy signal
If a provider repeatedly edits the same section, that is the training roadmap. Track edit type, not just edit volume. This is how teams move from “good scribe” to “elite scribe.”
Zone 7: “Plan without instructions”
If the plan does not tell the patient what to do, what to watch for, and when to return, you get rework. Scribes build plan clarity templates.
Zone 8: Handoff documentation
Referrals, follow ups, results review, and patient instructions are high risk. A scribe system makes these explicit and trackable.
For career positioning and proof, keep your outcomes measurable. If you want to show hiring managers your impact, connect your work to market demand insights in the job outlook report and regional opportunity guides like best cities for scribe careers.
4) The “Accuracy Engine”: a step by step system scribes use to keep quality high under pressure
If your clinic is serious about accuracy, build a repeatable engine. This is what separates a scribe who types fast from a documentation team that protects the organization.
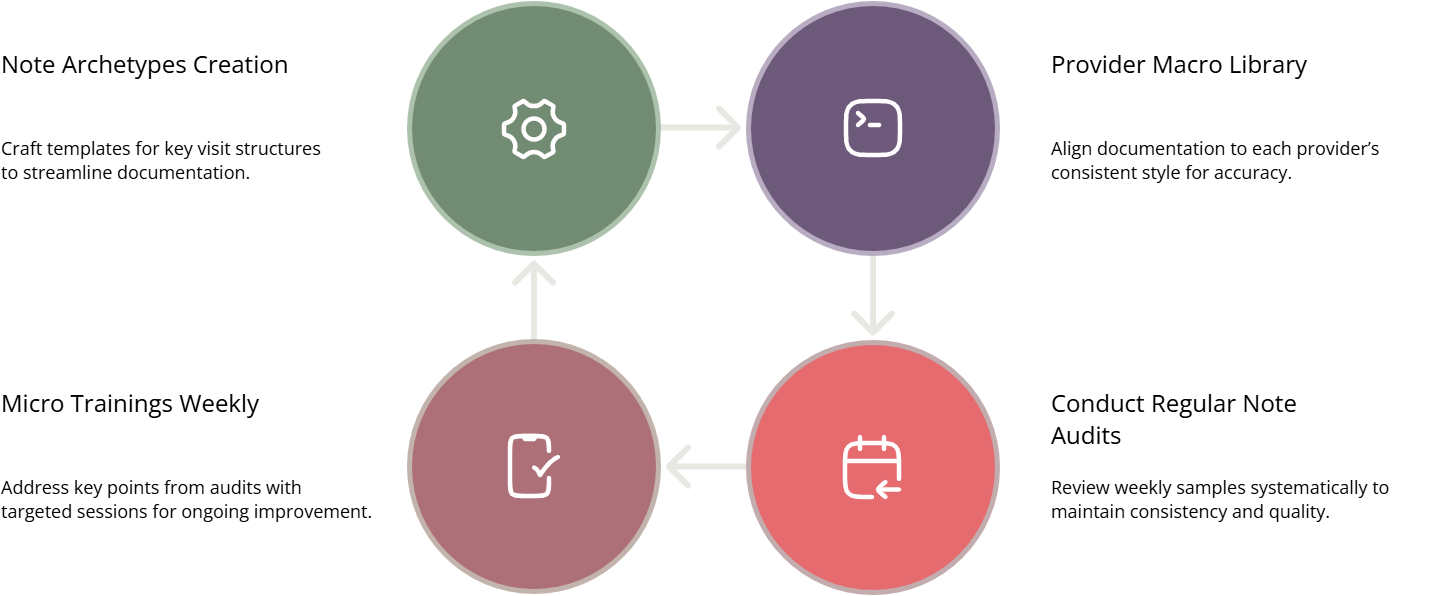
Step 1: Build note archetypes
Create 6 to 10 archetypes that cover the majority of visits. Examples: established follow up, acute complaint, chronic disease management, procedure visit, telehealth check in, results review. Each archetype has a template with:
Mandatory fields
“Prompt lines” that pull critical details
Safe phrasing for medical necessity and plan clarity
Telehealth and time blocks where needed
Step 2: Create a provider specific macro library
Accuracy improves when the scribe documents in the provider’s consistent voice. That reduces edits and prevents “meaning drift.” Track the top 20 repeated phrases the provider uses, then convert them into structured macros. This aligns with the “macro reuse” mindset that CMAAs use too. Explore adjacent software workflows in the EMR software terms guide and the admin systems angle in patient management systems.
Step 3: Run a weekly 20 note audit
You do not need a huge audit to move accuracy. You need consistency. Pull 20 notes per week across providers and visit types. Score them using the same rubric. Track the trend line.
If you want an example of how ACMSO frames performance outcomes across roles, compare operational metrics in the annual scribe salary and market report and the CMAA side through the CMAA salary report. Salary growth follows measurable value.
Step 4: Turn audit findings into “micro training”
Every week, pick one failure point and train it for 10 minutes. Examples: telehealth elements, assessment plan alignment, medication reconciliation prompts, specificity prompts. This keeps improvement continuous without slowing the clinic.
Step 5: Close the loop with denials, coding, and compliance
Accuracy is proven downstream. Pull denial reasons, coding queries, compliance findings, and patient callbacks. Map each issue back to a documentation failure point. Then update templates and scripts. This is how scribes become “documentation operators” instead of “note typists.”
You can also broaden your understanding of workflow friction by studying patient flow management terms and scheduling software concepts.
5) Proof that accuracy improved: the KPIs that make leadership take scribes seriously
If you want leadership buy in, stop saying “notes are better.” Show proof. Scribes can drive outcomes that are visible, measurable, and hard to argue with.
Here are the KPIs that matter most:
Provider edits per note and edit type trend
Time to close notes and sign off rate
Documentation completeness score from audit rubric
Coding query rate per 100 encounters
Denials related to documentation gaps trend
Telehealth compliance completion rate
Clarification calls and patient callbacks related to confusion
Problem list, allergy, medication reconciliation accuracy rate
Referral bounce backs and incomplete orders rate
If you want to position yourself for higher tier roles, connect documentation accuracy to career stories and market demand. Use the credibility anchors from success stories from scribes and the CMAA equivalents in CMAA success stories.
Also keep your career strategy aligned to where demand is growing. That is why interactive reports matter for targeting specialties and locations. Build your plan using the scribe job growth by specialty report and the admin equivalent in job demand by specialty.
Accuracy is not only skill. It is leverage. When you reduce rework and risk, you become expensive to replace.
6) FAQs
-
It should not mean “the note looks complete.” A strong definition breaks accuracy into scored components: correct patient story, correct medication and allergy data, correct assessment plan alignment, correct compliance elements, and correct coding support. Many clinics reach 90% plus when they measure accuracy weekly using a consistent rubric and when scribes run standardized capture prompts. If you want a practical model, build a weekly audit based on the same habits taught in the scribe exam preparation resources and reinforce it with repetition using the interactive practice exam.
-
Edits drop because the note becomes predictable, structured, and in the provider’s voice. Most edits are not about clinical disagreement. They are about missing specifics, unclear plan language, telehealth elements, or copy forward mistakes. A trained scribe anticipates these issues and captures the missing details in real time. The fastest way to reduce edits is to build a provider specific macro library and track edit type trends weekly. This aligns with the efficiency improvements described in research on scribe impact.
-
Yes, if the workflow is designed for it. Remote scribing fails when audio is poor, workflows are unclear, or telehealth compliance steps are not standardized. It succeeds when the team uses checklists, template archetypes, and consistent handoffs, and when the scribe has clear access to visit context. Remote teams should especially master telehealth documentation elements and time capture. If remote is part of your plan, study the operational shifts in remote scribing and the broader role changes in virtual medical administration.
-
The most dangerous mistakes are subtle: copy forward of old problems, medication list drift, missing rationale for orders, vague plans with no timelines, and telehealth notes missing required elements. These issues may not be obvious during the visit, but they show up later as denials, compliance exposure, and patient confusion. Scribes prevent them by using prompt macros and weekly audits. If you want to build this skill fast, sharpen your foundation with medical terminology mastery and tighten your exam level understanding through the exam breakdown guide.
-
Show trends, not opinions. Track provider edits per note, audit rubric scores, telehealth completeness, coding query rates, and denial reasons related to documentation. Run the same measurement weekly for 8 to 12 weeks, then present the before and after. Leadership responds to reduced rework and reduced risk. If you want to translate documentation impact into career value, connect it to market outcomes using the job market outlook and measurable business outcomes like those discussed in scribe revenue impact analysis.
-
Start with structured listening, clinical terminology, and “prompt discipline.” Structured listening means you can capture the patient story with timeline, context, and change. Terminology means you do not guess. Prompt discipline means you always verify medication, allergies, and plan timelines instead of assuming. Then build template control skills so you do not let default text override reality. If you want a roadmap, align your skill building with essential employer skills and avoid time wasting learning patterns in common exam mistakes.
-
A scribe does not make clinical decisions. They protect the documentation process. That means ensuring required elements are present, ensuring attestations match the visit type, ensuring telehealth documentation is complete, and ensuring time and consent elements are documented properly. The boundary is simple: the provider owns the clinical content and decisions, while the scribe owns the structure, completeness, and clarity of how it is recorded. For tech and workflow language that helps you operate cleanly, build system literacy using the EMR terms walkthrough and the admin workflow resources like patient flow management.