Patient Management Systems: Interactive Dictionary & Examples
Patient management systems are centralized digital platforms that streamline how healthcare providers handle appointments, medical records, billing, and communication. In 2025, they’ve become mission-critical tools—powering efficiency, patient safety, and financial sustainability across clinics, hospitals, and specialty practices. Whether you're onboarding staff or rethinking your infrastructure, understanding how these systems function is key to staying competitive and compliant.
This guide serves as your interactive, no-fluff reference, designed for healthcare administrators, clinicians, and operational teams. It defines the most essential patient management terms, breaks down core system functions, and delivers real-world use cases to show these tools in action. Each section is packed with practical examples, built to clarify how the right software elevates care quality, streamlines workflows, and reduces burnout. From intake forms to HIPAA audits, you'll walk away with a deeper, clearer understanding of how to apply these systems for immediate operational and clinical impact.
What Is a Patient Management System?
Core Definition & Role
A patient management system (PMS) is a software solution that consolidates the administrative, clinical, and financial operations of a healthcare facility. It integrates appointment scheduling, electronic medical records (EMRs), billing, insurance, and communication into one unified interface. These systems reduce fragmentation, eliminate redundant paperwork, and enable real-time access to patient data across departments.
More than just a tool, a PMS acts as the nerve center of clinical operations, ensuring that staff, patients, and stakeholders stay aligned. The result is measurable: faster patient throughput, lower administrative overhead, and improved care continuity. Nearly 92% of U.S. healthcare facilities now use integrated PMS solutions, a leap driven by digital transformation and compliance mandates.
Whether cloud-based or locally hosted, modern PMS platforms are built to scale—from solo practitioners to hospital networks—while maintaining data accuracy, regulatory alignment, and patient engagement at every level.
Scope in Modern Healthcare
The reach of patient management systems extends far beyond simple scheduling. In today’s hybrid care environments, PMS platforms facilitate multi-location coordination, integrate with telehealth modules, and automate billing cycles based on live service data. These platforms are also pivotal in managing chronic care, where patient follow-ups, medication tracking, and outcome reporting need to be synchronized across multiple providers.
They’re also foundational for value-based care delivery, offering tools for tracking patient satisfaction, engagement metrics, and clinical quality scores. As new care models like remote patient monitoring (RPM) and AI-assisted triage gain traction, PMS frameworks are adapting to support real-time data syncing, predictive analytics, and integrated alerts for high-risk cases.
Ultimately, the scope of a PMS is not just operational—it’s strategic. It informs decision-making, optimizes resource use, and ensures holistic continuity of care across all touchpoints.
Key Functions (Scheduling, EMR, Billing, etc.)
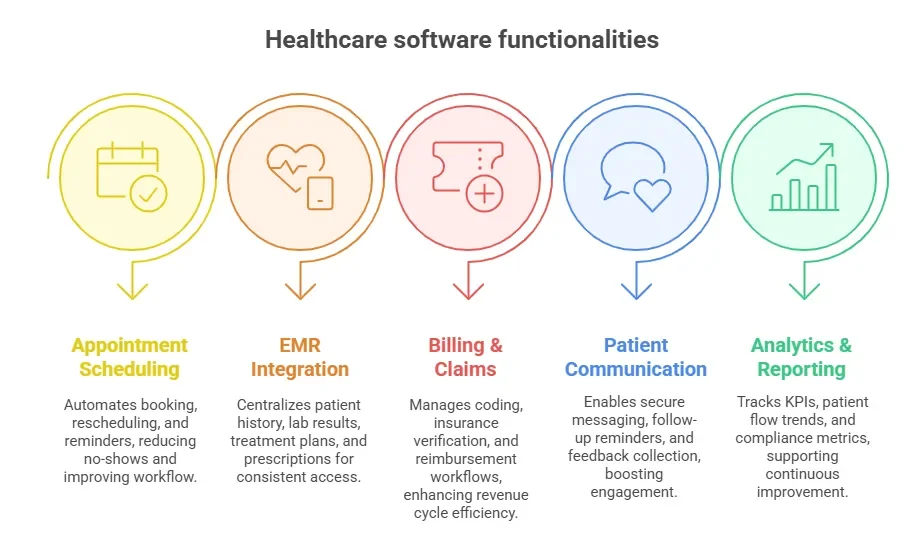
Most PMS platforms revolve around these essential modules:
Appointment Scheduling: Automates booking, rescheduling, and reminders. Reduces no-shows by up to 38%, according to industry benchmarks.
EMR Integration: Centralizes patient history, lab results, treatment plans, and prescriptions. Ensures all providers have consistent, real-time access to updated records.
Billing & Claims: Handles coding (ICD-10, CPT), insurance verification, and reimbursement workflows. Reduces errors and improves revenue cycle efficiency.
Patient Communication: Enables secure messaging, follow-up reminders, and feedback collection. Improves engagement while supporting HIPAA compliance.
Analytics & Reporting: Tracks operational KPIs, patient volume trends, and compliance metrics for continuous quality improvement and audit readiness.
Each module is designed to improve efficiency, compliance, and care delivery—not in isolation, but as an integrated system.
Why Clinics and Hospitals Rely on Patient Management Software
Boosting Administrative Efficiency
Patient management software eliminates manual bottlenecks by digitizing routine workflows—scheduling, charting, billing, and reporting—freeing staff to focus on high-impact tasks. Features like real-time calendar updates, automated patient reminders, and integrated billing modules allow front-desk teams to manage 30–40% more patients per day with fewer administrative errors.
Instead of juggling disparate spreadsheets or legacy tools, clinics now rely on centralized dashboards to manage patient intake, waitlists, and provider availability. This consolidation translates to faster decision-making, smoother shift transitions, and fewer missed entries. With interoperability across labs, pharmacies, and insurers, PMS solutions remove the need for repeat data entry—reducing delays, boosting throughput, and lowering labor overhead.
Enhancing Patient Experience & Outcomes
Modern patient management platforms are designed around patient-centric care. Patients can book appointments online, access records through secure portals, and receive reminders via SMS or email. This empowers them to manage their own care, increasing engagement and satisfaction scores across the board.
On the provider side, instant access to longitudinal patient data—medications, diagnoses, visit notes—supports more accurate clinical decisions. Fewer redundancies mean shorter wait times, faster diagnoses, and improved follow-up adherence. When PMS tools integrate with outcome tracking systems, they enable teams to monitor chronic conditions, flag abnormal results, and personalize care plans.
Ultimately, patient management software bridges the gap between operational efficiency and clinical quality, allowing organizations to do both—at scale.
Improving Compliance & Audit Readiness
Regulatory frameworks like HIPAA, MACRA, and MIPS have made airtight data handling a non-negotiable requirement. Patient management systems embed role-based access, audit trails, consent forms, and encryption protocols into their core, ensuring that every access point is traceable and defensible.
During audits, PMS platforms allow practices to quickly pull logs, track e-signatures, and demonstrate compliance across scheduling, documentation, and billing. Automated alerts flag incomplete records, expired credentials, or improper access—helping practices correct issues before they become violations.
Moreover, PMS analytics dashboards assist in tracking quality measures and performance incentives, ensuring eligibility for payer reimbursements and value-based care bonuses. With built-in compliance checks and documentation workflows, clinics are no longer scrambling before audits—they’re prepared by default.
Key Components of a Patient Management System
Appointment Scheduling & Reminders
Scheduling is more than time-slot assignment—it’s a critical front-end gateway that drives operational flow and revenue. PMS platforms offer real-time appointment syncing across departments, calendar automation, and smart triage features that assign patients based on urgency or provider specialty.
Integrated reminders via SMS, email, and push notifications can reduce no-shows by up to 38%, minimizing revenue loss and improving care continuity. Systems also allow for batch scheduling (ideal for flu shots, follow-ups, or multi-specialty visits) and last-minute cancellations to be filled instantly, maximizing daily capacity utilization.
Some platforms even use machine learning to predict high-risk cancellations and offer double-booking safeguards to minimize schedule gaps. These tools turn appointment coordination into a predictable, streamlined engine rather than a chaotic variable.
Patient Records & EMR Integration
Patient data sits at the heart of care. PMS platforms offer direct integration with Electronic Medical Records (EMRs) to ensure seamless documentation, instant retrieval, and multi-provider access. Every lab result, radiology report, and progress note is unified into a chronological timeline, minimizing errors and boosting decision accuracy.
Advanced record modules support SOAP note formatting, interoperability with diagnostic systems, and real-time syncing with wearable devices and remote monitoring tools. Providers gain the ability to annotate, flag anomalies, and review full medical histories before patient arrival—all from one screen.
This connected data ecosystem reduces fragmentation while supporting faster, safer care—especially in emergency or multi-specialist settings where decision time is critical.
Billing, Insurance, and Claims
Billing workflows have long been prone to errors and delays. Modern PMS platforms automate insurance verification, eligibility checks, preauthorization tracking, and claims submission, dramatically reducing rejected or denied claims.
Coding tools built into the system suggest ICD-10 or CPT codes based on chart entries, flag mismatches in real time, and allow batch claim processing for payers. These tools accelerate reimbursement cycles, ensure compliance with payor-specific requirements, and generate financial reports for reconciliation.
The inclusion of patient wallets and e-payment portals further streamlines the revenue cycle. With integrated billing tools, practices gain transparency, accuracy, and control over their financial lifelines.
Analytics & Reporting Tools
Every interaction—from check-in to payment—is logged as structured data. Built-in analytics tools convert this data into dashboards showing no-show rates, patient flow trends, billing lags, and compliance metrics. These insights power strategic decisions: staffing needs, operational changes, or resource allocation.
Customizable reports help administrators track key performance indicators (KPIs), detect patient attrition patterns, and ensure targets for regulatory quality measures (e.g., HEDIS, UDS) are met. These tools are essential for organizations participating in value-based care models or accountable care organizations (ACOs).
At their best, PMS platforms don’t just record activity—they reveal insights that transform care delivery and business growth.
| Component | Function & Value |
|---|---|
| Appointment Scheduling & Reminders | Offers real-time syncing, automated reminders, batch scheduling, and machine-learning prediction of no-shows. Helps reduce missed appointments by up to 38% and improves operational flow. |
| Patient Records & EMR Integration | Ensures seamless documentation and real-time access to lab results, visit notes, and patient history. Supports faster decision-making and minimizes errors, especially in multi-specialist environments. |
| Billing, Insurance, and Claims | Automates verification, coding (ICD-10/CPT), and claims processing. Reduces denials, improves compliance, and enhances revenue cycle control with built-in e-payment tools. |
| Analytics & Reporting Tools | Transforms structured patient data into dashboards and reports for tracking KPIs, patient trends, and compliance metrics. Drives strategic decisions and supports value-based care success. |
Patient Management Dictionary – Most Important Terms
Front Office Terms
Intake Forms: Digital or paper-based questionnaires that capture key patient data at the time of registration—demographics, medical history, allergies, and insurance. PMS tools allow auto-population of these forms, reducing front-desk time and improving data accuracy across departments.
Insurance Verification: A critical pre-visit step where eligibility and benefits are confirmed with the payer. Integrated verification modules within PMS systems can perform real-time checks, reducing claim denials and pre-visit uncertainties.
Walk-In Management: Systems that accommodate unscheduled visits without disrupting existing appointments. PMS software enables real-time queue updates, average wait-time tracking, and load-balanced provider assignment for efficient handling of walk-ins without patient churn.
These terms power the first impression and operational flow of any clinic—high-functioning front offices rely on automation to reduce chaos and improve throughput.
Clinical Terms
SOAP Notes: Structured documentation format capturing Subjective, Objective, Assessment, and Plan. PMS systems often embed this directly into EMRs for faster charting and standardized clinical workflows.
EHR (Electronic Health Record): The longitudinal digital file containing the patient’s full clinical history. EHRs integrated within PMS platforms allow instant access across departments, supporting continuity of care, chronic disease tracking, and timely decision-making.
Encounter Documentation: Detailed logs of each visit, including vitals, symptoms, diagnoses, procedures, and treatment plans. Accurate documentation is essential for legal protection, billing compliance, and performance audits under value-based care models.
Understanding these clinical inputs ensures teams maintain documentation quality, consistency, and legal defensibility.
Billing & Admin Terms
ICD-10: International classification system for diseases. PMS systems auto-suggest codes during documentation, improving billing accuracy and claims success rates.
CPT: Current Procedural Terminology codes used to describe medical procedures. PMS solutions embed these into charge capture systems, reducing coding errors and supporting real-time revenue tracking.
Preauthorization: Payer-required approval before conducting certain procedures. Integrated modules monitor preauth status and automate submission, ensuring care is not delayed and claims are not denied.
Co-Pay: The fixed patient-paid portion at the point of service. PMS tools calculate co-pays dynamically and enable seamless collection via POS or patient portals, improving front-desk cash flow.
Admin and billing terms shape how care gets funded and documented, making them essential to sustainable practice operations.
Compliance Terms
HIPAA (Health Insurance Portability and Accountability Act): Governs patient data privacy and security. PMS platforms are required to offer encryption, access logs, and secure user authentication to remain HIPAA compliant.
Audit Trail: A timestamped log of every user interaction with the system—who accessed what, when, and why. Enables accountability, forensic tracing, and regulatory transparency.
Role-Based Access: Permission controls that limit system functions by user type—e.g., front desk, physician, billing. These access rules protect patient privacy and system integrity, especially in multi-user settings.
Compliance isn’t optional—these terms define legal survivability in a digital healthcare landscape.
| Front Office Terms | Clinical Terms | Billing & Admin Terms | Compliance Terms |
|---|---|---|---|
| Intake Forms: Questionnaires collecting demographics, history, and insurance. PMS tools auto-fill data, reducing front-desk workload. | SOAP Notes: Standardized documentation (Subjective, Objective, Assessment, Plan) embedded into EMRs. | ICD-10: Diagnostic coding system. PMS auto-suggests codes for accurate billing. | HIPAA: Regulates patient data privacy. PMS includes encryption, access logs, and secure login. |
| Insurance Verification: Confirms coverage before visit using real-time PMS checks, reducing denials. | EHR (Electronic Health Record): Full clinical history accessible across departments via PMS integration. | CPT: Procedure codes embedded into PMS for real-time charge capture and billing accuracy. | Audit Trail: Timestamped user logs supporting accountability and regulatory transparency. |
| Walk-In Management: Tools for handling unscheduled visits using queue updates and provider balancing. | Encounter Documentation: Detailed visit notes including symptoms, procedures, and plans; critical for audits. | Preauthorization: Required insurer approval before procedures. PMS tracks and automates requests. | Role-Based Access: Access control by role to maintain system integrity and patient confidentiality. |
Examples of Patient Management Systems in Action
Solo Practice – Efficiency Boost
A one-provider family medicine clinic in suburban Texas adopted a cloud-based PMS to solve three key problems: missed appointments, slow billing, and charting delays. With just one physician and one front-desk staff member, time was scarce—and errors were costly.
By implementing an integrated platform with automated appointment reminders, real-time insurance verification, and SOAP note templates, the clinic reduced no-shows by 31% within 60 days. Front-desk workload dropped significantly as patients completed digital intake forms via patient portals before arriving.
The physician now finishes daily notes before leaving the office—thanks to auto-filled fields and speech-to-text features—eliminating hours of after-hours charting. Claims are submitted electronically with real-time CPT and ICD-10 validation, cutting down on billing rejections.
In short, this PMS transformed a paper-heavy, reactive practice into a data-driven, patient-ready system without adding staff or expanding hours. The ROI showed within 90 days—more billable encounters, shorter wait times, and better patient reviews.
Multi-Specialty Clinic – Integration Case
A multi-specialty clinic with internal medicine, dermatology, cardiology, and radiology struggled to manage patient data across its various departments and satellite labs. Manual processes led to repeated tests, missed follow-ups, and fragmented patient care.
The solution was a PMS built with interoperable EMR integration, allowing specialists to view shared patient charts in real time. Radiology results and lab reports now sync automatically to the referring provider’s dashboard, while dermatologists can tag chronic cases for long-term treatment tracking.
Pharmacy orders, imaging requests, and referral workflows are now routed digitally through the same system—eliminating redundant paperwork and boosting interdepartmental collaboration. Patients can view test results, refill medications, and confirm appointments through a unified portal.
After implementation, the clinic reported a 22% reduction in redundant diagnostics and a 19% improvement in follow-up adherence within six months. Communication between providers improved, and average wait times per patient dropped by seven minutes.
The PMS didn’t just connect systems—it created a frictionless care experience across multiple disciplines, maximizing both efficiency and patient trust.
Hospital System – Scaling Up
A 400-bed regional hospital faced major scalability issues—departmental silos, communication delays, and audit risks were undermining clinical outcomes. Discharges were routinely delayed due to medical billing and documentation backlogs.
By deploying an enterprise-grade PMS with HL7 compatibility, the hospital unified its departments—emergency, surgery, ICU, pharmacy, radiology, and billing—under one digital infrastructure. Discharge summaries, medication orders, and provider handoffs are now synchronized in real time.
The billing chain was automated with real-time coding suggestions, insurance cross-checks, and error-flagging tools. The discharge process, once a 6–8 hour ordeal, now takes less than 2 hours. Clinical teams use task dashboards and secure internal messaging to manage care handoffs, reducing miscommunication events by nearly 40%.
Audit preparedness also improved. Administrators can generate compliance logs, track user access, and flag anomalies instantly through role-based reporting tools. With 12 departments now aligned, the hospital turned its PMS into a clinical command center, improving care coordination and revenue cycle management at scale.
| Setting | Challenges Before PMS | Solutions Implemented | Results & Outcomes |
|---|---|---|---|
| Solo Practice | Missed appointments, delayed billing, after-hours charting; 1 physician + 1 front-desk staff | Cloud-based PMS with reminders, insurance checks, SOAP templates, and voice-to-text charting | 31% no-show reduction; faster charting; fewer errors; increased billable visits; improved patient reviews |
| Multi-Specialty Clinic | Data fragmentation across internal med, derm, cardio, radiology; repeated tests and poor coordination | PMS with interoperable EMR, shared dashboards, synced lab/radiology/pharmacy data | 22% fewer redundant tests; 19% better follow-up rates; faster communication; 7-minute average wait time reduction |
| Hospital System (400-bed) | Department silos, delayed discharges, audit risks, manual billing chain | Enterprise PMS with HL7, real-time task dashboards, billing automation, and access control | Discharge time cut from 6–8 hrs to <2 hrs; 40% fewer miscommunications; full audit traceability; system-wide alignment |
How Patient Management Tools Support Medical Scribe Certification by ACMSO
Application in Real-World Clinical Settings
Patient management systems are core to the role of medical scribes—especially those trained through the Medical Scribe Certification by ACMSO. These professionals are responsible for live clinical documentation, data entry, and workflow support across high-volume care settings.
PMS platforms provide scribes with structured interfaces to:
Capture real-time SOAP notes during provider-patient interactions
Access previous encounters, medication histories, and diagnostic reports instantly
Streamline communication between providers, labs, and billing teams via internal messaging modules
Graduates of the Medical Scribe Certification by ACMSO are trained to navigate EMR systems, but PMS tools add a broader layer of integration—connecting clinical documentation with scheduling, billing, and compliance oversight. This ensures scribes input notes in the right templates, with the correct coding support, and without duplication or omissions.
In hospital or specialty clinic settings, scribes use PMS dashboards to queue up patient lists, pre-load documentation templates, and manage encounter timelines—improving provider efficiency by up to 33%. Features like voice-to-text dictation, ICD-10/CPT code suggesters, and audit logs also reduce post-shift charting burdens for physicians.
Scribes certified by ACMSO are uniquely positioned to become indispensable members of care teams, supporting workflow optimization and EHR compliance through skilled use of patient management software. Their mastery of both the clinical language and digital tools directly improves chart accuracy, billing speed, and provider satisfaction.
Frequently Asked Questions
-
A patient management system (PMS) is a comprehensive platform that includes appointment scheduling, billing, insurance verification, reminders, and communication. An EMR (Electronic Medical Record), on the other hand, specifically refers to the digital version of a patient's clinical chart. While EMRs focus on storing clinical data like vitals, diagnosis, and treatment notes, PMS tools offer a broader operational scope—including non-clinical functions vital for running a practice. Many modern platforms integrate EMRs into the PMS framework, ensuring seamless access to both administrative and clinical workflows. For medical scribes, understanding this integration is essential to streamline documentation, prevent errors, and support full-spectrum care delivery across departments.
-
Patient management systems provide a structured environment that helps medical scribes quickly access patient charts, preload documentation templates, and record real-time clinical encounters. Features like SOAP note fields, voice dictation tools, and auto-fill templates reduce manual input and speed up documentation. PMS dashboards often allow scribes to see upcoming patient queues and prioritize documentation based on visit type and complexity. Integrated ICD-10 and CPT suggesters help scribes align notes with billing codes, improving reimbursement accuracy. By mastering PMS platforms, certified medical scribes can cut physician documentation time by over 30%, contributing directly to improved care efficiency and provider satisfaction.
-
Yes. Patient management software significantly reduces billing errors by integrating real-time insurance verification, code validation, and claims submission tools. As scribes enter documentation, the system cross-references notes with CPT and ICD-10 codes, flagging mismatches or missing fields. Preauthorization tracking ensures that services requiring prior approval are not delayed or billed inappropriately. PMS tools also log every billing-related action, creating an audit-ready documentation trail. This level of automation minimizes the risk of denials and improves the speed of revenue cycle management. Trained medical scribes using these systems help create more accurate notes, ensuring clean claims and faster payment processing.
-
Outpatient clinics benefit from PMS features that improve patient throughput, reduce no-shows, and streamline coordination across departments. Key modules include: real-time appointment scheduling, automated reminders, EMR access, integrated billing, and patient communication tools. For clinics with specialty providers, multi-provider scheduling and telehealth support are also crucial. PMS tools allow staff to track average wait times, no-show rates, and billing performance in a single dashboard. Medical scribes in outpatient settings use the platform to manage encounter logs, preload forms, and ensure timely documentation completion. These tools support faster patient turnover, reduced provider burnout, and more accurate reporting.
-
Yes. The Medical Scribe Certification by ACMSO includes training in navigating Electronic Medical Records and patient management systems commonly used in outpatient and hospital settings. Students learn how to input SOAP notes, retrieve patient histories, work with ICD-10/CPT codes, and follow clinical workflows that align with EHR and PMS platforms. The curriculum emphasizes real-world usability—training scribes to recognize documentation priorities, compliance risks, and workflow optimization opportunities. Familiarity with PMS tools prepares graduates to work across specialties, improving their hiring potential and performance in fast-paced clinical environments where documentation accuracy and speed are critical.
-
Patient management systems ensure compliance through role-based access, encryption, e-signature tracking, and automatic audit logs. Each user interaction is timestamped and traceable, ensuring accountability. PMS platforms also house consent forms, intake data, and medical records in structured formats aligned with HIPAA and regulatory guidelines. In case of an audit, administrators can generate reports showing documentation trails, preauthorization logs, and coding histories. For medical scribes, this means every note they document becomes part of a compliant, verifiable record. Mastering PMS software allows scribes to support legal, regulatory, and insurance-related documentation without needing to manually manage or cross-check compliance standards.
-
Yes, depending on the employer’s infrastructure and compliance policies, medical scribes can use cloud-based PMS platforms to document encounters in real-time from remote locations. Telemedicine and remote care models have expanded the scope for virtual scribing, especially in specialties like psychiatry, dermatology, and internal medicine. Secure, HIPAA-compliant platforms allow scribes to join patient visits virtually, capture notes directly into EMRs, and sync with billing and scheduling teams. The key is ensuring access controls, encryption, and provider-supervised workflows. Scribes trained through the Medical Scribe Certification by ACMSO are equipped to navigate these platforms efficiently—whether on-site or remote.
-
An EMR (Electronic Medical Record) is the digital version of a paper chart used in one clinic. An EHR (Electronic Health Record) includes a broader view of a patient’s care across multiple providers and facilities. A PMS (Patient Management System) covers administrative operations—scheduling, billing, reminders, and messaging. Most modern systems integrate all three. Medical scribes primarily work within the EMR/EHR portion to capture visit notes, vitals, and diagnoses. However, scribes trained through the Medical Scribe Certification by ACMSO also use PMS features like encounter logs, ICD/CPT suggestions, and patient lists. Understanding how these systems intersect is critical to real-time documentation and workflow optimization.
Final Thoughts
Mastering patient management systems is no longer optional—it’s a competitive edge. From intake to discharge, every step of patient interaction is logged, scheduled, billed, and tracked through these platforms. Understanding how they work means understanding how modern healthcare truly operates.
For those pursuing or holding the Medical Scribe Certification by ACMSO, fluency in patient management systems translates into immediate value on clinical floors. It means faster documentation, fewer provider errors, and a more efficient workflow that impacts both revenue and patient safety. Certified scribes who excel in PMS platforms are not just assistants—they become essential collaborators in the care process.
This guide gave you more than just definitions—it gave you real applications, live examples, and the technical fluency needed to work smarter in any care setting. From front desk lingo to audit trail mechanics, you now understand the language of patient flow.
Healthcare is evolving fast. The ability to interpret, use, and improve systems like these sets you apart—whether you’re on your first day as a scribe or scaling a multisite operation. Invest in the systems, master the terms, and you’ll master the future of clinical efficiency.