Medical Billing Software: Essential Terms & Interactive Tutorials
Medical billing software has evolved from static data entry to intelligent claim management tools that dictate reimbursement success. Whether you're preparing for the CPC or CPB certification, or streamlining workflows in a live practice, mastering the exact terminology these systems use is critical. Misunderstanding even a single field—like Payer ID or 837 files—can trigger claim denials, compliance flags, or lost revenue. Every click in a billing system reflects a regulation or reimbursement rule.
Interactive tutorials now mimic real-world billing cycles, helping learners practice CPT/ICD-10 coding, claim scrubbing, and rejections resolution. Instead of memorizing disconnected terms, professionals gain hands-on experience through simulated claims, AI coding prompts, and alerts that reinforce accuracy. These tools aren’t just nice to have—they bridge the gap between theory and operations. In this guide, we break down the essential language, mistake-proof training tools, and certification-ready platforms that give billing pros a competitive edge.
Essential Medical Billing Software Terminology
Claim Lifecycle Language
Claim accuracy begins with knowing how each form, field, and file fits into the reimbursement process. One of the most essential terms is the 837 file—the digital format used to submit claims to payers. A billing error here doesn’t just cause delays; it prevents the claim from even reaching the insurer. Then there’s the EOB (Explanation of Benefits), which outlines what the payer covered, denied, or adjusted. Misinterpreting it often leads to missed appeals and patient misbilling.
The superbill, often created by the provider, includes CPT and ICD codes that define the services rendered. But when front-desk staff or coders misunderstand its structure, mismatches with the patient’s chart or insurance plan cause immediate denials. The clearinghouse, meanwhile, acts as a filter—converting, checking, and routing claims. If a denial occurs here, it’s not always due to bad coding; it could be formatting errors, invalid payer IDs, or even missing provider NPIs.
Every term in the lifecycle is tied to a risk or opportunity. Failing to understand the difference between claim rejections at the clearinghouse and denials from the payer delays follow-ups. CPC and CPB candidates must know how these terms apply to real claims—not just definitions, but how, where, and why they trigger specific downstream effects. Interactive tutorials that walk learners through a full billing cycle—from patient encounter to payer response—make the difference between theoretical familiarity and operational fluency.
Technical & Interface-Level Terms
Behind every claim interface are backend protocols that make data move accurately and securely. One such protocol is HL7 (Health Level 7)—used for exchanging clinical and administrative data between systems like EHRs and billing software. It doesn't impact how a coder enters data, but it determines whether the claim file pulls correct patient and service info. An incomplete HL7 message can mean submitting a claim with the wrong provider or encounter date.
EDI (Electronic Data Interchange) is another foundational term—referring to the electronic transmission of healthcare documents, especially claims. Claims aren’t simply emailed; they’re packaged in EDI formats that systems like clearinghouses and payers can interpret. Any mismatch in structure can corrupt the file. Payer ID, a numeric routing code, ensures the claim reaches the right insurance company. Submitting with a wrong or outdated ID—something tutorials regularly simulate—leads to complete processing failure.
NPI (National Provider Identifier) is more than a credentialing number—it’s tied to your reimbursement rights.** Submitting claims without a matching NPI can void the entire batch. Tutorials that walk users through NPI mapping, payer ID selection, and HL7 setup are essential—not just for coders but for anyone working in billing compliance or claims submission.
Software training that incorporates these backend elements ensures learners know what’s under the hood. The best tutorials show where these terms live in claim forms, how to troubleshoot mismatches, and what logs or reports to check when something goes wrong. Without hands-on exposure to these technical elements, certification candidates struggle with simulation exams and real job performance.
| Term | Definition |
|---|---|
| 837 File | A standardized digital file used to submit medical claims to payers. |
| EOB (Explanation of Benefits) | A document from the payer detailing what was covered, denied, or adjusted in a claim. |
| Superbill | A provider-generated form listing CPT and ICD codes for services rendered. |
| CPT Codes | Procedure codes used to describe medical, surgical, and diagnostic services. |
| ICD Codes | Diagnosis codes used to classify diseases and conditions for billing. |
| Clearinghouse | A third-party system that checks, converts, and routes claims to the appropriate payer. |
| Claim Rejection | A claim that fails initial checks (e.g., format errors) and is not accepted for processing. |
| Claim Denial | A claim that is received by the payer but not reimbursed due to issues like eligibility or medical necessity. |
| NPI (National Provider Identifier) | A unique 10-digit number identifying healthcare providers in all administrative transactions. |
| Payer ID | A numeric code used to route claims to the correct insurance payer. |
| CPC (Certified Professional Coder) | A certification for individuals who specialize in coding medical services for billing. |
| CPB (Certified Professional Biller) | A certification for individuals who manage the revenue cycle, including claims and reimbursement. |
| HL7 (Health Level Seven) | A standard for exchanging electronic healthcare data between systems like EHRs and billing platforms. |
| EDI (Electronic Data Interchange) | The electronic transmission of structured healthcare data, especially for submitting claims. |
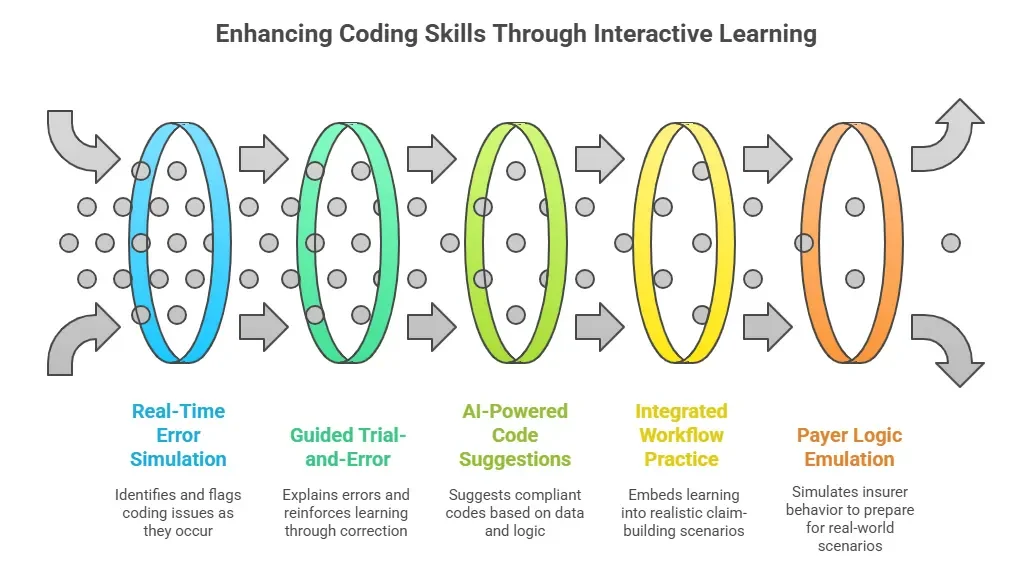
Interactive Features That Actually Teach
Claim Scrubbers and Alerts
Claim scrubbers do more than catch typos—they replicate how payers flag reimbursement risks in real time. When you input a CPT code without the correct modifier, scrubbers throw an alert before submission. For instance, submitting 99213 with a procedure code but no modifier may bypass your eye but not the scrubber. Tutorials that simulate this live—flagging before sending—train coders to develop an autopilot instinct for coding integrity.
AI-aided validation enhances this by suggesting probable code corrections based on past claims. The best software doesn’t just tell you an ICD-10 code is off—it offers a suggested replacement based on specialty, patient demographics, or payer guidelines. It mimics payer logic to a point where learners start thinking like a denial management team.
These systems reinforce learning through guided trial and error. The alert doesn’t just show a red flag; it explains what caused it—missing NPI, invalid date range, modifier mismatch. And this isn’t just useful in practice—it maps directly to CPB and CPC exam prep, which increasingly includes claim auditing simulations.
Tutorials that embed these tools within workflow simulations produce deeper retention. Passive learners become active troubleshooters. Instead of reading a paragraph about “modifier -25,” they learn it when the system halts a submission without it. This is where most online billing courses fall short—they talk about claim logic but don’t simulate its enforcement.
Coding Assist and Predictive Tools
Modern platforms now guide coders toward accurate choices in real time. Coding assist tools suggest CPT and ICD-10 codes based on keywords, documentation, or past patterns. For example, typing “diabetic foot ulcer” triggers a shortlist of compliant ICD-10 codes, often with payer-specific suggestions. These predictive engines reduce lookup time, prevent common mismatches, and boost confidence—especially for new coders.
Predictive features go further by auto-matching diagnoses to services. In integrated systems, choosing a procedure like 11042 (debridement) prompts ICD suggestions like L97.421 or E11.621, depending on the context. When tutorials replicate these features, learners begin to see the logic of reimbursement unfold live.
Speed matters too. In real-world billing, coders often handle 40–60 claims per day. Predictive tools reduce friction, eliminate redundant searches, and help avoid undercoding. Tutorials that force learners to use these tools—rather than merely reading about them—accelerate skill acquisition. Especially for CPC certification, where time management under coding pressure is tested, these features simulate that high-speed reality.
Leading billing platforms like AdvancedMD, Kareo, and DrChrono embed these learning aids into user training modes. Tutorials expose learners to predictive assist in actual billing scenarios—completing a chart, resolving an alert, finalizing a scrubbed claim. When education happens inside a workflow, memory retention spikes.
The best tutorials don’t just demonstrate features—they require the user to act. Pick a code. Respond to a prompt. Choose the right payer. And when they’re wrong? The system explains why, in context. This is the training that builds operational readiness—not just test-taking familiarity.
Avoidable Mistakes Learners Make (and How Tutorials Help)
Code Level Selection Errors
One of the most costly beginner mistakes in medical billing is choosing the wrong level of service. This often results in upcoding, where the claim implies a higher complexity than actually documented, or downcoding, where the reimbursement is lower than it should be. Both can trigger payer audits or revenue loss. Tutorials that simulate this decision-making—asking learners to assign CPT levels based on chart notes—train better instincts.
Static PDFs or lectures can’t replicate the nuance of real coding decisions. For example, differentiating between 99213 and 99214 depends on time, complexity, and documentation. Interactive tutorials present patient scenarios and force the learner to pick a code, then justify it. Immediate feedback helps solidify the correct thresholds and avoids guesswork that becomes a liability on the job.
Certification exams like CPC and CPB require more than memorization—they demand situational judgment. Learners who’ve only read about code ranges struggle when tested on real-world modifiers or MDM (medical decision-making). Tutorials that use actual visit notes and live coding tools are vastly superior to passive study methods.
Tutorials also help learners recognize over-reliance on “safe codes.” Some new coders default to broad or vague ICD-10 codes because they’re afraid of errors. But this creates a pattern of undercoding, which hurts revenue and analytics. Guided tutorials provide a safe space to make, review, and correct mistakes with no downstream risk.
Misunderstanding Rejections
Not all billing rejections are the same—and beginners often fail to identify their root cause. Clearinghouse rejections happen before the claim reaches the payer and are usually due to formatting issues: invalid NPI, wrong payer ID, or incorrect EDI structure. Payer denials, by contrast, relate to clinical or policy-based issues, like coding mismatches or eligibility problems. Tutorials that walk learners through rejection reports are essential for making this distinction.
Many beginners miss the retry workflow entirely. After a clearinghouse rejection, the corrected claim must be re-queued, not just resubmitted blindly. If tutorials don’t force the user to fix and resubmit the claim manually, learners skip this step altogether in real life—leading to aging claims, cash flow delays, and missed deadlines.
The right tutorials teach learners how to read and respond to remittance reports. Instead of scanning EOBs for check amounts, learners should be taught to dissect adjustment codes, reason codes, and remark codes. Interactive platforms like SimClaim or AAPC’s billing practice modules offer walkthroughs where users trace a claim’s full journey—submission, rejection, correction, and final approval.
Understanding this lifecycle is crucial for passing certification exams and succeeding in entry-level roles. Coders must know what to look for and how to act when a claim bounces back. Tutorials that show the full loop, not just the front end, create billing pros who solve problems instead of escalating them.
| Learner Mistake | Why It Happens | How Tutorials Help |
|---|---|---|
| Wrong Code Level Selection | Confusion between CPT levels (e.g., 99213 vs 99214) due to lack of clinical context | Simulates real patient notes, forces code selection with feedback |
| Over-Reliance on “Safe” Codes | Fear of errors leads to vague, non-specific coding | Promotes confident ICD selection through safe, guided experimentation |
| Undercoding for Simplicity | Assumes lower codes are safer, which reduces reimbursement | Demonstrates revenue impact of habitual undercoding |
| Guessing Without Justification | Memorization-based learning fails in practical scenarios | Tutorials require justification for each coding decision |
| Not Understanding Rejections | Learners can’t distinguish clearinghouse vs payer issues | Walkthroughs show rejection types, fixes, and re-submission process |
| Skipping Re-Queue Steps | Lack of familiarity with clearinghouse retry workflow | Simulated rejections require manual correction and re-submission |
| Ignoring Adjustment Codes | Learners focus on check amounts, not denial reasoning | Interactive reports teach how to read and respond to EOB details |
| Fragmented Lifecycle Knowledge | Learners only see claim creation—not rejection, correction, and approval stages | End-to-end simulations trace the claim from submission to resolution |
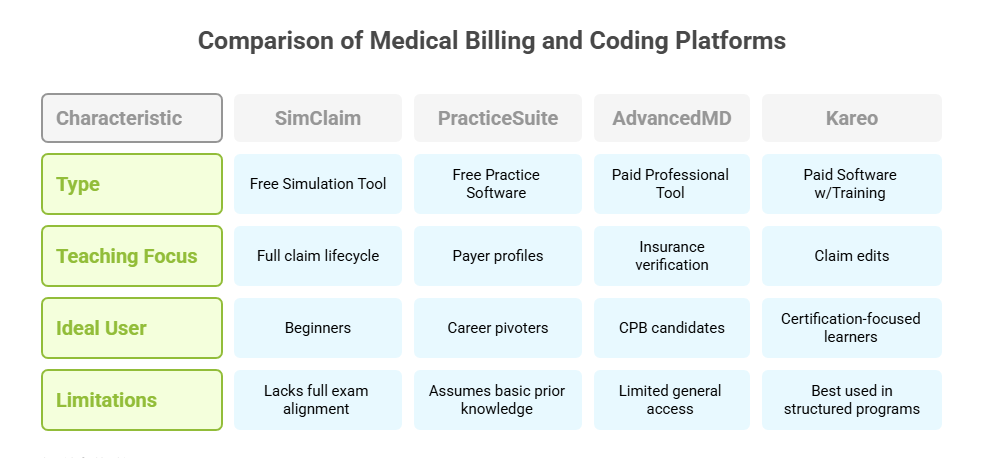
Best Free and Paid Tools for Training
Beginner-Friendly Practice Platforms
Learning medical billing starts faster—and smarter—with hands-on simulation tools. Platforms like SimClaim and PracticeSuite offer structured billing practice for new coders, covering everything from basic demographics entry to ICD/CPT pairing and claim submission. These tools are ideal for those preparing for certification or pivoting into healthcare admin roles.
SimClaim stands out by offering a full mock claim cycle—from patient visit to payment status. Learners are walked through form fields, submission options, and even clearinghouse error prompts. It’s especially useful for understanding the timing and order of operations, which most textbooks skip.
PracticeSuite provides real-world context by including multiple payer profiles and role-specific dashboards. This helps users experience what it’s like to work as a front-office biller, coding analyst, or A/R specialist. However, its tutorials are not as guided as SimClaim, making it better suited for learners who already have foundational knowledge.
These platforms offer cost-effective exposure, but they’re limited in feedback and exam alignment. Most lack full coverage of AAPC test objectives or fail to simulate real denial management. They’re excellent starter tools, but not a full prep solution. Use these tools for muscle memory and foundational workflows—but plan to supplement with certification-aligned platforms if you're targeting professional-level accuracy or high CPC/CPB exam scores.
Professional Software with Built-In Training
The fastest way to learn billing software is inside the actual platforms used by clinics and billing services. Tools like AdvancedMD and Kareo come with training sandboxes—safe environments where learners can create, edit, and submit mock claims using live interfaces.
AdvancedMD’s training mode includes guided modules on insurance verification, claim creation, and rejection resolution. Each module reflects real workflows, meaning the interface learners see is identical to what they’ll encounter on the job. It’s especially helpful for CPB candidates, as it mimics payer communications, secondary billing logic, and real remittance handling.
Kareo offers built-in learning paths with milestone tracking. Learners are shown how to set up billing templates, attach proper codes, and correct common errors flagged by scrubbers. Its visual prompts and guided decision trees make it easier for beginners to learn without supervision.
What sets these tools apart is their alignment with real operational billing. You’re not just simulating a claim—you’re building it inside the same platform used in thousands of practices across the U.S. This translates directly into career-readiness. However, access is usually limited to students enrolled in programs or internships. Those outside professional education tracks may need to use demo versions or pay for licensed access. But for learners serious about mastering billing, these tools are worth the investment.
Real-World Applications for CPC + CPB Certification
Exam-Aligned Tutorial Tools
Passing the CPC or CPB exam isn’t just about knowing codes—it’s about applying them in real billing scenarios. That’s why interactive tools designed around AAPC objectives are now integral to serious prep. Simulations that walk users through coding a full visit—from diagnosis to billing—are proven to boost accuracy and confidence under test conditions.
Tutorials like those from AAPC or embedded within tools like Medesk or Kareo simulate real workflows tied to exam topics. Learners aren’t just quizzed on CPT ranges—they’re asked to resolve denials, correct claims, and apply coding guidelines to multi-step problems. This reinforces decision-making under pressure, just like the timed format of the CPC exam.
The best tools go beyond rote drills by mimicking interface logic, payer edits, and modifier use. These functions train students to think like working coders, not just test takers. When a claim gets rejected, learners must fix it—not skip it—mirroring real-world expectations.
If you’re preparing for certification without using workflow-based simulations, you’re leaving points on the table. The exams increasingly favor case-based scenarios and process awareness—tutorials must match that structure to deliver results.
How Practice Builds Career Readiness
Real-world billing success depends on more than memorized code sets—it demands full-cycle training. Top certification programs now include tutorials that mimic intake, eligibility check, coding, submission, and denial follow-up. These aren’t just helpful—they’re essential for entry-level readiness.
Practice labs that walk you through the entire revenue cycle help connect the dots. Learners move from a patient chart to code selection, claim formatting, and payer follow-up—all in one scenario. This builds fluency in the end-to-end process, the kind employers expect even from fresh hires.
These simulations also expose learners to crucial soft skills. For example, navigating a real-time rejection message teaches not just technical troubleshooting, but accountability and urgency. The repetition of fixing live errors builds a mindset of resolution rather than escalation.
For CPB candidates especially, hands-on exposure to claim edits, patient balances, and appeal workflows is a must. Tutorials that simulate these steps don’t just prepare you for the exam—they show you how to succeed the moment you’re hired. That’s why certification-backed tools with full practice workflows aren’t optional anymore—they’re the new standard.
How ACSMO’s Certified Scribes Are Trained to Navigate Medical Billing Software Like Pros
ACSMO’s Certification is built around interactive learning—not passive reading. Every module includes claim lifecycle walkthroughs, automated alerts, and guided correction labs that reflect real-world payer logic. Instead of just teaching what a CPT or ICD-10 code is, ACSMO tutorials show learners how codes function across an actual reimbursement chain.
Learners follow real claim examples—from patient intake through denial resolution—inside platform-based simulations. These labs use mock EMR systems and billing dashboards to reinforce software fluency. For example, one module may ask learners to submit a claim using 99214 and ICD-10 code E11.9, then prompt them to respond to a scrubber alert when the modifier is missing.
Each workflow is broken down into step-by-step simulations that mirror both CPC and CPB-level expectations. Students handle eligibility checks, payer matching, scrubber warnings, and final submission—all within one practice session. Every misstep triggers immediate in-context feedback, allowing users to correct and resubmit without guesswork. This closes the theory-to-execution gap that traditional courses fail to address.
ACSMO’s Certification also includes guided rejections management tutorials. When a clearinghouse flags a formatting error or an NPI mismatch, learners are taught to trace the error back to source, correct it, and push the updated claim forward. This cycle-based repetition builds confidence and competency—critical for exam readiness and job performance.
Unlike static videos or basic quizzes, ACSMO’s training tools are built around performance tasks. Learners must apply knowledge in motion—choose codes, submit claims, analyze errors, and follow payer logic. This is where ACSMO stands apart: it trains billing professionals the way they’ll actually work.
All tutorials and workflow simulations are integrated into the full curriculum. This central hub provides lifetime access to realistic billing environments, claim tracking scenarios, and exam-ready practice modules. For learners serious about mastering the billing cycle—and passing industry exams—this certification offers more than content. It delivers operational skill. Every click, correction, and completion reinforces how professional billing operates in the real world.
Frequently Asked Questions
-
Start with terms directly tied to claim flow: 837 files, superbill, EOB, clearinghouse, payer ID, and NPI. These aren’t just technical labels—they control whether a claim is accepted, denied, or delayed. If you misunderstand where to enter an NPI or which payer ID applies, your entire submission can fail. Most claim software also uses HL7 and EDI formats, so you’ll need to recognize how these interact with your billing platform. Learning them first creates a solid workflow foundation and reduces your error rate during both certification exams and real practice. Use interactive tutorials that show these terms inside forms, not just as definitions.
-
Interactive tutorials force you to do the task—not just read about it. Instead of memorizing how a claim is submitted, you actually fill one out, fix alerts, and respond to denials. This turns passive recall into active understanding. The best platforms provide immediate feedback when errors occur, helping you correct mistakes in real-time. Tutorials also mimic payer edits, scrubber logic, and EOB responses, giving you an immersive environment that mirrors actual billing jobs. This accelerates confidence and makes you exam-ready faster than static courses. Simulation-based training also improves long-term retention by up to 40%, based on multiple industry reports.
-
Claim scrubbers, AI-assisted coding, payer rule libraries, and real-time eligibility checks are key. Scrubbers catch common coding errors—like missing modifiers or expired policy numbers—before the claim ever reaches the payer. AI features suggest CPT/ICD pairings based on visit notes, ensuring the codes match the documentation. Some tools also include denial reason simulators or historical denial analysis, which help you adjust codes pre-submission. When these features are built into tutorials, they also teach you the logic behind denials. Mastering these tools doesn’t just reduce your rejection rate—it helps you understand how payers think, which directly supports ACSMO Certification readiness.
-
Yes—SimClaim and PracticeSuite both offer limited-access tools ideal for beginners. SimClaim lets you walk through entire claims, including eligibility, coding, and submission, using realistic workflows. PracticeSuite offers a more expansive platform, with basic tutorials on insurance entry, claim forms, and EOB matching. However, free tools often lack feedback mechanisms, scrubber simulations, or live error correction. They’re useful for initial exposure but won’t be enough for full ACSMO exam prep. That’s why pairing a free tool with a structured program—like ACSMO’s Certification—is ideal. The combination gives you both skill practice and guided progression that leads to certification-level competency.
-
Clearinghouse rejections happen before the claim reaches the insurer. They usually stem from format errors, like a missing NPI, invalid dates, or a non-existent payer ID. These claims never even make it to the insurance company. Payer denials, by contrast, occur after the claim has been accepted and reviewed by the payer. They’re based on policy rules—like coding mismatches, non-covered services, or eligibility issues. Tutorials that show both scenarios—often with editable claims—help learners develop the skill to troubleshoot, fix, and resubmit without delay. Knowing the difference prevents confusion, ensures faster revenue cycles, and is a key ACSMO prep topic.
-
Coding assist tools reduce human error and speed up submissions by auto-suggesting CPT/ICD-10 codes based on diagnoses or documentation. For instance, typing “diabetes” might pull up E11.9 and suggest procedure codes depending on the chart context. These tools often factor in payer rules, specialties, or even past submission history. In tutorials, learners are exposed to these tools and taught how to vet the suggestions rather than blindly accept them. This not only prevents denials but trains learners to recognize valid coding logic. They’re especially useful for newer professionals who are still learning the depth and nuance of medical code sets.
-
Yes, ACSMO’s Certification is designed to support both beginners and those transitioning into healthcare billing from adjacent roles. The course includes interactive tutorials, real-world billing labs, live error simulations, and exam-style walkthroughs. Learners don’t need prior coding experience; the curriculum gradually builds from foundational terms to complex claim troubleshooting. Tools like claim scrubbing, modifier logic prompts, and rejection management are integrated into the training. The result is a course that mirrors on-the-job expectations while preparing you for the exam with guided precision. Lifetime access and step-by-step instruction ensure you’re never left behind, even if you’re starting from zero.
Final Thoughts
Learning medical billing software isn’t just about passing a test—it’s about mastering the tools that define your value in any healthcare role. Whether you're entering the field or pursuing ACSMO’s Certification, you need to speak the language of claim lifecycles, scrubber alerts, payer logic, and clearinghouse protocols. Every denial avoided and every claim approved on the first try begins with technical fluency.
Interactive tutorials are the single most effective way to build this fluency. They embed knowledge through action—letting you see, correct, and reapply billing logic in real time. That skill transfers directly to job performance and exam readiness. If you're serious about advancing in this field, you can't afford to learn billing software passively.
ACSMO’s Certification delivers exactly what the market demands—hands-on, workflow-based training that prepares you for both employment and compliance audits. In today’s reimbursement-driven healthcare systems, your billing knowledge is your leverage. Make sure it’s earned through tools that teach the way real billing operates.