EMR Software Terms: Interactive Dictionary & Walkthroughs
Electronic Medical Records (EMR) systems are the digital backbone of modern healthcare, used daily by physicians, coders, nurses, and admin staff. But despite being mission-critical, most users interact with only a small fraction of what EMRs are capable of—primarily because the terminology itself creates a learning wall. Terms like “CPOE,” “flowsheets,” and “FHIR” are tossed around in clinics and training sessions, but few professionals know exactly what they mean or how they affect workflow, billing, or compliance.
This guide is your hands-on dictionary and walkthrough—designed not just to define EMR software terms but to show you how they work inside real clinical roles. You’ll get deep clarity on core functions, compliance-critical fields, and interactive features used in platforms like Epic, Cerner, and eClinicalWorks. Whether you’re aiming for faster charting, fewer billing errors, or higher compliance scores, understanding these terms changes everything. And if you're ready to practice what you learn, we’ll also show you how to use our ACSMO certification to simulate real-world use cases and turn theory into immediate skill.
Core EMR Terminologies You Need to Know
Understanding EMR systems starts with decoding the foundational terms that shape every clinical interaction, billing entry, and administrative task. These aren’t just “nice to know”—they’re essential for anyone aiming to streamline patient care, ensure documentation accuracy, and meet regulatory demands. Below, we break down three of the most important terminology clusters: system modules, documentation tools, and interoperability protocols.
Clinical vs Administrative Modules
EMR platforms divide functionality into two broad categories: clinical modules and administrative modules. Clinical modules handle patient-centered tasks like charting, medication administration, lab integration, and decision support. Administrative modules, on the other hand, focus on scheduling, billing, insurance verification, and performance reporting.
Understanding which module governs a task helps eliminate documentation errors and ensures that data is captured in the right context. For instance, inputting vitals under a billing tab could create downstream issues in coding or audit compliance. EMRs like Epic and Allscripts distinctly separate these modules to maintain clarity across teams. Mastering the module structure improves cross-functional collaboration and reduces friction between clinical and administrative workflows.
Charting, Templates, and Encounters
Charting refers to the act of recording a patient’s medical information within the EMR. Most systems allow for template-driven charting, which preloads standardized fields based on specialty or visit type. This improves speed, consistency, and regulatory adherence. “Encounters” are the containers for these interactions—each time a patient is seen, a new encounter is logged with its own date, location, and reason for visit.
Well-designed templates reduce free-text errors, support faster billing cycles, and increase clinical throughput. Customizable templates can include smart phrases, dropdowns, and prefilled data—helping providers spend more time on care and less on screens. Every entry inside an encounter—from vitals to procedures—is timestamped and audited.
HL7, FHIR, and Integration Layers
Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) are the two primary data exchange standards that allow EMRs to talk to other health systems. HL7 is widely used for messaging between systems—like pushing lab results from a diagnostic platform into the EMR. FHIR, on the other hand, focuses on modular, API-based access that makes real-time data sharing more efficient and secure.
Understanding these standards is vital when working with interface engines, third-party apps, or analytics dashboards. Without HL7 or FHIR integration, your EMR becomes a silo—unable to push or receive critical clinical data. EMRs that offer flexible integration layers empower organizations to adopt telehealth, remote monitoring, and AI diagnostics without starting from scratch.
| Term | Definition |
|---|---|
| Charting | Recording a patient’s clinical data within the EMR. |
| Medication Administration | Documenting medications prescribed and given to patients. |
| Lab Integration | Importing lab results directly into the EMR system. |
| Clinical Decision Support | Tools that offer evidence-based guidance during clinical decision-making. |
| Scheduling | Managing appointments, provider availability, and room allocation. |
| Billing | Recording charges and generating claims for services rendered. |
| Insurance Verification | Confirming a patient’s insurance eligibility and coverage. |
| Performance Reporting | Generating metrics and reports on clinical or operational performance. |
| Templates | Predefined documentation forms tailored to visit type or specialty. |
| Smart Phrases | Prewritten text shortcuts for faster data entry. |
| Dropdowns | Selectable lists used for standardized documentation. |
| Prefilled Data | Automatically populated patient data fields based on previous records. |
| Encounters | Each unique visit or interaction with a patient, documented in the EMR. |
| Vitals | Measured physiological data such as blood pressure, heart rate, etc. |
| Procedures | Documented clinical interventions performed during a patient visit. |
| HL7 (Health Level Seven) | A standard for transmitting healthcare data between software systems. |
| FHIR | A modern, API-based standard for real-time, secure health data exchange. |
| Interface Engines | Middleware systems that manage and translate data between different health IT systems. |
| Third-Party Apps | External software tools integrated into EMRs for added functionality. |
| Analytics Dashboards | Visual platforms that display real-time insights from EMR data. |
| Telehealth Integrations | EMR extensions that support virtual consultations and remote care. |
| Remote Monitoring Tools | Devices or software that collect and send patient data from outside clinical settings. |
| AI Diagnostics | Artificial intelligence tools embedded in EMRs to assist in analyzing clinical data. |
Workflow & Documentation Terms Explained
EMR software isn’t just a storage system—it’s a workflow engine. The way notes are categorized, orders are processed, and actions are logged can either accelerate patient care or introduce costly delays and risks. This section breaks down core documentation terms that directly affect clinical clarity, audit compliance, and operational efficiency.
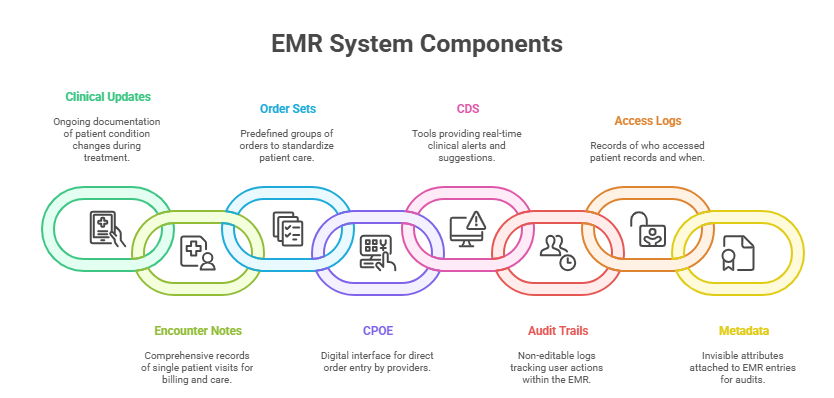
Progress Notes vs Encounter Notes
Though often used interchangeably, progress notes and encounter notes serve distinct functions in EMRs. Progress notes are daily updates or sequential entries made during a patient’s ongoing treatment. They capture changes in condition, lab follow-ups, or status updates.
Encounter notes, however, are comprehensive records tied to a single visit or interaction. They include subjective and objective data, provider assessments, diagnoses, and plans. Each encounter note typically triggers billing and coding workflows—making accuracy critical.
Confusing the two can lead to incomplete documentation, missed codes, or compliance red flags. Knowing the difference improves continuity of care, ensures proper handoffs, and minimizes duplicate entries across disciplines.
Order Sets, CPOE, and Clinical Decision Support
Order sets are predefined bundles of tests, meds, or procedures based on specific clinical scenarios. For instance, an order set for chest pain may include ECG, cardiac enzymes, and aspirin. These sets standardize care and reduce errors.
Computerized Physician Order Entry (CPOE) is the mechanism through which providers place these orders in the EMR. CPOE is often integrated with Clinical Decision Support (CDS) tools, which offer real-time alerts, contraindication warnings, or treatment guidelines.
Used correctly, these tools drive evidence-based medicine, reduce variation, and flag dangerous interactions before harm occurs. Misuse or over-alerting, however, can cause alert fatigue, which leads clinicians to ignore even critical prompts.
Audit Trails, Access Logs, and Metadata
Every action within an EMR—viewing a chart, editing a note, prescribing meds—is logged in the audit trail. This non-editable log captures who did what, when, and from where. Access logs are part of the audit structure but focus specifically on who accessed patient records, which is key for HIPAA compliance.
Metadata refers to the invisible data tied to every entry: timestamps, user IDs, device types, and even screen resolution. In audits or legal reviews, this metadata is often what determines whether a record was tampered with or not.
Understanding these back-end logs is crucial not just for compliance officers—but also for clinicians, administrators, and IT teams aiming to catch misuse early and ensure record integrity.
Compliance-Critical Vocabulary in EMRs
Healthcare isn’t just about documentation—it’s about documenting correctly, legally, and securely. EMRs are built to align with strict regulatory frameworks, but only if the users understand how those rules are enforced within the software. These are the terms that directly influence legal defensibility, patient privacy, and audit outcomes.
HIPAA, 21 CFR Part 11, and OHRP
HIPAA (Health Insurance Portability and Accountability Act) governs how patient data is stored, accessed, and shared. In EMRs, HIPAA compliance means enforcing access controls, audit logging, encryption, and secure messaging. Every EMR user must understand that even accidental disclosures—like leaving a screen open—can be violations.
21 CFR Part 11 applies mainly to clinical trials and electronic records regulated by the FDA. It demands that systems ensure data integrity, audit trails, and electronic signature validation—all built into EMRs used in research settings.
OHRP (Office for Human Research Protections) sets policies on how patient data is handled in federally funded research. If your EMR connects with research databases, understanding these frameworks becomes essential for IRB approval and study integrity.
Consent Management, eSignatures, and Authentication
Consent management refers to capturing, storing, and updating patient permissions for treatment, data sharing, or participation in research. EMRs typically allow forms to be signed digitally, tracked over time, and linked to patient encounters.
Electronic signatures (eSignatures) are bound by both HIPAA and e-sign laws like the E-SIGN Act. These signatures must be uniquely attributable, time-stamped, and locked post-signing. Whether it’s an informed consent or discharge summary, a valid eSignature is a legal safeguard.
Authentication refers to how users are verified within the system. It can range from simple passwords to two-factor login, biometric scans, or badge swipes. Role-based authentication restricts access so that clinicians only see what they need, and nothing more.
Data Retention & Archival Protocols
Healthcare data can’t just be deleted when it’s old. EMRs must follow data retention laws that vary by country, state, and use case. For example, pediatric records may need to be stored for at least 21 years, depending on jurisdiction.
Archival protocols define how inactive records are stored. Most EMRs offer cold storage solutions or offloaded backup systems, ensuring records remain intact but don’t consume active system resources. Understanding retention policies is critical for avoiding legal risks, insurer denials, or record loss.
| Term | Definition |
|---|---|
| HIPAA | U.S. regulation that governs patient data privacy, access controls, audit trails, and secure information exchange in EMRs. |
| 21 CFR Part 11 | FDA rule that applies to electronic records in clinical trials; requires audit trails, electronic signatures, and data integrity. |
| OHRP | Office that oversees human research protections; regulates how EMRs manage research data tied to federally funded studies. |
| Consent Management | The process of digitally capturing and updating patient permissions for treatment, data use, or research participation. |
| eSignatures | Legally binding electronic signatures that must be attributable, time-stamped, and locked post-signing for audit protection. |
| Authentication | Verification method for EMR users, including passwords, biometrics, or two-factor authentication, often role-based. |
| Data Retention | The legal requirement to store patient data for a defined period based on jurisdiction and patient type (e.g., pediatric). |
| Archival Protocols | The policies and technologies used to store inactive medical records securely while preserving access for legal or clinical needs. |
Interactive Elements in EMRs: What They Actually Do
Modern EMRs aren’t just digital filing cabinets—they’re dynamic interfaces built to drive faster decision-making, reduce error rates, and surface critical information in real time. Knowing how to interpret and use interactive elements can elevate your clinical accuracy and administrative efficiency.
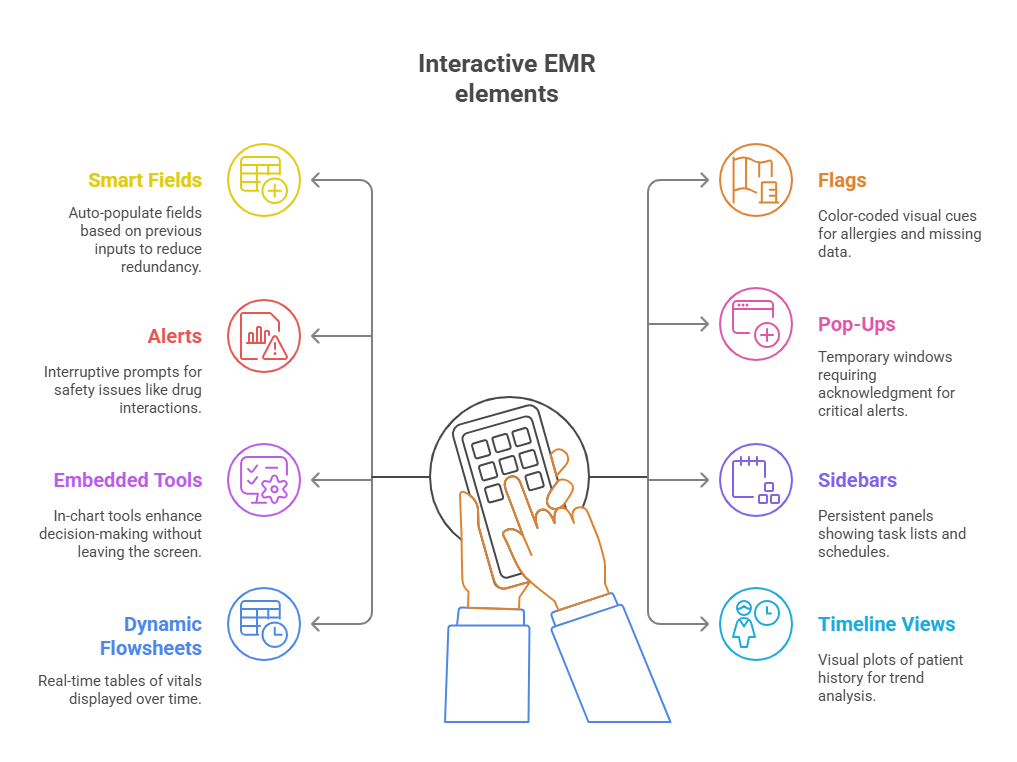
Smart Fields, Flags, and Alerts
Smart fields are data-driven entry points that auto-populate based on prior entries, patient context, or templates. For example, entering a diagnosis of diabetes might auto-suggest A1C testing in adjacent fields. These dynamic inputs minimize redundancy and reduce clicks.
Flags are visual indicators—often red, yellow, or green—used to mark allergy status, missing documentation, or urgent tasks. They’re configurable and user-specific, helping clinicians identify issues without digging through multiple tabs.
Alerts are interruptive messages triggered by specific actions or omissions. These include medication interaction warnings, duplicate order notices, or missing vital signs. When designed properly, alerts enhance clinical safety—but excessive or poorly configured alerts lead to alert fatigue, decreasing effectiveness.
Pop-Ups vs Embedded Tools vs Sidebars
Pop-ups are temporary windows that demand action or acknowledgment—often used for critical alerts, consent forms, or reminders. While effective for urgent communication, they risk interrupting clinical flow if overused.
Embedded tools live within the charting interface itself. These can include coding assistants, risk calculators, or quality metric checklists. Because they’re integrated, they support real-time decision support without requiring users to leave the primary workflow.
Sidebars are persistent panels on the edge of the screen. They offer continuous access to task lists, schedule queues, or communication threads. Unlike pop-ups, sidebars remain visible but non-intrusive—ideal for multi-tasking environments.
Dynamic Flowsheets and Timeline Views
Dynamic flowsheets present structured clinical data—like vitals, labs, and medication history—across a time axis. Unlike static PDFs or printouts, these flowsheets update live and allow users to sort, filter, or compare values instantly.
Timeline views offer visual plots of patient history, encounters, procedures, and medication adherence. Some EMRs integrate interactive sliders or icons that let you zoom in on hospitalization events, trends, or post-discharge issues. These tools are essential for pattern recognition and long-term care planning.
The more fluently you use these interactive components, the more confidently you’ll navigate patient records, spot red flags, and accelerate your documentation speed—while staying fully compliant.
EMR System Configurations for Admin Staff
While clinicians focus on charting and diagnostics, administrative staff rely on EMRs to streamline scheduling, billing, access control, and task coordination. EMRs offer a wide range of configuration tools that directly impact practice performance, claims processing, and data governance. Understanding these features is key to reducing inefficiencies and ensuring regulatory compliance from the admin side.
Role-Based Access and Security Groups
Role-based access defines what each user can view, edit, or delete based on their job function. For instance, a front-desk staff member might only have access to demographics and scheduling, while a coder can view diagnosis fields but not clinical notes.
Security groups are predefined permission bundles applied across user roles. These ensure that access policies remain consistent, auditable, and easy to update as teams evolve. Misconfigured roles can lead to data breaches, HIPAA violations, or accidental record tampering.
Understanding how to assign, modify, and review permissions helps reduce both internal risks and external audit failures. It also supports faster onboarding for new hires—getting them up to speed without compromising security.
Billing Code Mapping, CPT/ICD-10 Plugins
Admin teams are responsible for ensuring that the clinical documentation supports proper billing. EMRs often offer built-in plugins or integration layers for CPT (Current Procedural Terminology) and ICD-10 (diagnostic) coding. These tools translate chart entries into billable units, validate coding logic, and flag discrepancies in real time.
Some platforms allow custom code mappings—connecting internal procedure names to CPT equivalents. Others offer auto-suggestion tools based on templates or diagnoses, reducing manual lookup time and coder fatigue.
Using these tools accurately impacts reimbursement speed, claim approval rates, and downstream reporting. Coders and billers who understand EMR-integrated coding workflows are consistently more productive.
Schedule Views, Color Coding, and Task Queues
Administrative efficiency often starts with the calendar. EMRs offer customizable schedule views that sort by provider, room, appointment type, or urgency. Color coding is used to visually tag appointment categories—e.g., red for urgent, green for follow-ups, blue for new patients.
Task queues route administrative responsibilities (like form verification, follow-up calls, or insurance checks) to the appropriate team members. These tasks can be auto-generated from appointment types or completed forms, and they ensure nothing slips through the cracks.
Mastering these configurations can shave hours off daily admin work, reduce bottlenecks, and keep patient flow optimized without sacrificing compliance or clarity.
| Function Area | EMR Tools / Configurations | Administrative Impact |
|---|---|---|
| User Permissions | Role-based access, security groups | Reduces data breaches, ensures HIPAA compliance, supports fast onboarding |
| Billing Workflow | CPT/ICD-10 plugins, billing code mapping, auto-suggestion tools | Improves claim accuracy, accelerates reimbursement, minimizes coder fatigue |
| Scheduling Efficiency | Custom schedule views (by provider, room, urgency), color coding | Enhances calendar clarity, reduces double-booking, streamlines provider load |
| Task Coordination | Task queues tied to forms, appointment types, or manual routing | Ensures accountability, prevents task omissions, supports workflow automation |
Learn EMR Software Terms Through Our Certification (ACSMO)
You’ve learned the key EMR terms—but knowing isn’t the same as doing. That’s why the ACSMO Certification goes beyond textbook definitions and lets you work directly inside simulated EMR environments. From clinical workflows to backend configurations, ACSMO’s program bridges the gap between theory and applied skill, giving you hands-on command of the exact tools and terms you’ll use on the job.
Interactive EMR Simulations
Each module in the ACSMO certification includes realistic EMR simulations—not screenshots or static walkthroughs. You’ll complete exercises like entering clinical notes through CPOE, updating consent forms, customizing user roles, and building documentation templates inside a functioning mock system.
You’ll learn to modify flowsheets, audit access logs, trigger alerts, and map ICD-10 and CPT codes as if you were in a live environment. These tasks are embedded within platform-based practice zones that reflect how real EMR systems like Epic and Cerner operate.
You won’t just define terms—you’ll perform them.
Certification Outcomes & Job Role Readiness
Graduates of ACSMO’s certification are prepared to step into EMR-heavy roles across clinical operations, administration, compliance, and informatics. The program equips you to:
Operate within structured EMR workflows
Implement role-based access settings with audit compliance
Conduct documentation reviews and flag inconsistencies
Manage encounter and chart-level actions with full accuracy
This isn’t general theory. It’s built for real job functions, giving you confidence to contribute immediately in healthcare teams where EMRs dominate daily workflows.
Who This Is Best For
This certification is ideal for:
Healthcare professionals transitioning into admin or EMR coordination roles
Medical coders, billers, and auditors who need EMR fluency
Health IT graduates preparing for system analyst or informatics jobs
Practice administrators looking to streamline team workflows
There’s no clinical license required. If you’re committed to mastering EMRs and becoming a go-to systems expert, the ACSMO certification delivers targeted, simulation-based training with career-ready outcomes.
Frequently Asked Questions
-
The most critical EMR terms include encounter, progress note, CPOE, audit trail, order sets, FHIR, and HL7. These terms affect everything from documentation speed to billing compliance and legal defensibility. “Encounter” refers to a single patient visit; “progress notes” are sequential updates. CPOE (Computerized Provider Order Entry) streamlines orders electronically, while audit trails track who accessed or edited records. FHIR and HL7 are data standards that support system interoperability. Without a clear understanding of these terms, it’s easy to misdocument care, create coding errors, or miss alerts. Mastery of this vocabulary enables faster workflows, higher accuracy, and safer handoffs between providers and departments.
-
EMR templates pre-structure documentation fields based on visit type, specialty, or workflow—saving time and standardizing entries. Smart fields take it a step further by auto-populating content based on context, diagnosis, or prior inputs. For example, selecting “Type 2 Diabetes” may auto-suggest A1C labs and dietary notes. These tools reduce typing, eliminate redundancy, and improve documentation speed by over 30% in many clinical settings. They also support coding accuracy by aligning charting with billable elements. When used properly, templates and smart fields ensure consistency, minimize manual errors, and make documentation audits significantly easier. They’re foundational tools in every modern EMR.
-
HL7 and FHIR are the backbone of EMR interoperability. HL7 (Health Level Seven) is used for structured data messaging between systems—like pushing lab results or scheduling info. FHIR (Fast Healthcare Interoperability Resources) uses web-based APIs for real-time access to patient data across platforms. Together, they allow hospitals, clinics, and external labs to share and receive information securely. Without HL7/FHIR literacy, clinical staff often face broken integrations, incomplete records, and data silos. Understanding how these protocols function helps healthcare teams troubleshoot delays, comply with federal mandates, and work more efficiently with third-party tools, including telehealth or billing platforms.
-
CPOE (Computerized Provider Order Entry) is the EMR feature that allows clinicians to electronically order labs, imaging, prescriptions, or procedures. It replaces handwritten orders, ensures structured entry, and reduces transcription errors. CDS (Clinical Decision Support) is a layer on top of CPOE that provides real-time guidance—such as drug-allergy alerts, dosage checks, or evidence-based treatment suggestions. CPOE executes the order; CDS advises or corrects it. These systems often work together but serve different roles: one captures actions, the other improves their quality. Understanding the distinction helps providers use both effectively, boosting patient safety and improving treatment consistency.
-
Audit trails track every action taken within the EMR—what was viewed, edited, or deleted—along with timestamps, user IDs, and device details. Metadata embedded in the audit trail ensures that records are legally defensible and compliant with regulations like HIPAA and 21 CFR Part 11. If there’s a dispute, investigation, or breach, the audit trail reveals who accessed what, when, and from where. This protects both the organization and the patient. In routine operations, it helps detect unusual access patterns, supports performance reviews, and flags unauthorized data usage. Audit trail literacy is essential for admins, managers, and compliance officers.
-
Absolutely. Healthcare admin roles—from front-desk coordinators to coding specialists—increasingly require fluency in EMR systems. Understanding EMR terms like role-based access, order sets, metadata, and templates can give applicants a significant hiring edge. It shows you’re not just familiar with clerical tasks—you’re ready to work within regulated systems and avoid costly mistakes. Employers prioritize staff who can document accurately, navigate systems independently, and spot errors before they escalate. Learning EMR terminology isn’t just resume filler—it’s a signal that you’re job-ready and can contribute immediately without a steep learning curve.
Final Thoughts
EMR fluency is no longer optional—it’s a core job skill across clinical, administrative, and IT roles in healthcare. Whether you’re a frontline provider, billing coordinator, or compliance lead, understanding EMR software terms directly impacts your workflow speed, documentation quality, and ability to avoid costly mistakes. It’s the difference between navigating confidently and constantly second-guessing every click.
This guide has broken down the most essential EMR terminology in a format that’s practical, not theoretical. But if you’re serious about turning that knowledge into career leverage, ACSMO’s certification takes you the rest of the way. With real EMR simulations, CPD-accredited lessons, and job-focused outcomes, you’ll gain hands-on mastery that hiring teams trust.
The healthcare industry is evolving fast—and EMR systems are evolving with it. The professionals who learn to master them, not just use them, will lead the next wave of high-impact, digitally fluent healthcare teams.
| Which EMR feature do you find most essential for administrative efficiency? | |
|---|---|