Conflict Resolution in Medical Admin: Interactive Dictionary
In medical administration, conflict resolution isn’t just about managing workplace disagreements—it’s a critical competency shaping patient outcomes, regulatory compliance, and operational efficiency. When disputes arise over resource allocations, team dynamics, or interdepartmental miscommunications, the ripple effects can compromise not only staff productivity but also patient safety and satisfaction. Addressing these conflicts proactively is vital to ensure smooth workflows and mitigate risks that could escalate into legal or reputational challenges.
Healthcare settings are high-pressure environments where precision matters. From managing medical records to coordinating multidisciplinary care teams, admin professionals face complex scenarios that demand clear communication and conflict resolution skills. Without structured protocols, even minor misunderstandings can trigger cascading delays, billing errors, or compliance failures. By mastering conflict resolution in medical admin, organizations can protect against regulatory breaches, improve service delivery, and foster a culture of collaboration.
Understanding Conflict Resolution in Medical Admin
Why Conflict Resolution is Critical in Medical Admin
Conflict resolution in medical administration is a cornerstone of healthcare operations. Every administrative decision—whether it involves scheduling, billing, or regulatory documentation—affects both patient outcomes and interdepartmental dynamics. When conflicts escalate unchecked, they disrupt workflows, compromise patient safety, and can even result in financial penalties due to compliance breaches. Medical administrators are tasked with mitigating these risks through clear, actionable strategies.
Conflicts often stem from role ambiguity, unclear communication, or resource constraints. When administrators fail to resolve these issues swiftly, backlogs form, treatment plans stall, and stress levels rise. This isn’t merely an internal challenge—it’s a systemic one that affects the hospital or clinic’s ability to deliver seamless care. Conflict resolution empowers staff to navigate these challenges effectively, aligning processes with both regulatory requirements and patient care goals.
Proactive conflict management improves morale, reduces turnover, and ensures operational continuity. It transforms healthcare facilities into environments where administrative efficiency and patient well-being coexist. Skilled administrators not only solve disputes—they preemptively identify triggers, de-escalate tensions, and implement standardized solutions to avoid recurring issues.
The Key Drivers of Conflict in Healthcare Settings
Several drivers fuel conflict in medical administration, and understanding them is essential for resolution:
Resource Scarcity: Competition for limited staff, equipment, or time creates friction. Misaligned expectations about priorities often fuel disagreements.
Communication Breakdowns: Inefficient information flow between departments or unclear documentation creates misunderstandings that escalate conflicts.
Regulatory Complexity: Navigating ever-changing compliance requirements introduces stress and errors, causing conflicts over responsibilities or interpretations.
Workload Disparities: Uneven task distribution can lead to resentment and burnout, making conflict inevitable.
Cultural or Interpersonal Differences: Diverse teams bring unique perspectives but can also experience misunderstandings without proper conflict management protocols.
Identifying and addressing these drivers is the first step toward building a resilient, conflict-ready medical admin structure.
Key Terms and Concepts
Essential Conflict Resolution Terms
Mastering conflict resolution in medical administration begins with understanding key terms that define resolution frameworks, communication protocols, and compliance considerations. These terms form the foundation for proactive, structured, and efficient conflict management in high-pressure environments:
Escalation Protocol: A predefined pathway for resolving conflicts that exceed standard administrative solutions, minimizing disruption.
Root Cause Analysis (RCA): A structured method for identifying underlying factors that contribute to recurring conflicts. It promotes sustainable resolution strategies.
Mediation: A facilitated process where a neutral third party assists conflicting parties to reach a mutually acceptable solution. It’s often used in disputes involving billing or patient care responsibilities.
De-escalation Techniques: Communication strategies designed to reduce tension and prevent escalation, crucial for handling emotional or high-stakes disputes.
Nonviolent Communication (NVC): An approach focusing on empathetic engagement and clarity in communication, ensuring discussions remain constructive.
Compliance Alignment: Ensuring conflict resolution strategies adhere to healthcare regulations like HIPAA, to prevent legal complications.
Each term integrates into daily admin workflows to ensure clarity, speed, and effectiveness in resolving conflicts while maintaining regulatory compliance.
How These Terms Apply in Daily Admin Workflows
In daily healthcare administration, these terms are more than definitions—they’re operational tools:
Escalation protocols ensure that unresolved issues don’t halt patient care or administrative operations. For instance, if a dispute arises over medical coding, an escalation pathway involving billing and compliance officers can resolve the issue swiftly.
Root Cause Analysis enables teams to go beyond surface-level disagreements. If recurring conflicts over resource allocations persist, RCA identifies system flaws rather than blaming individuals.
Mediation can defuse interpersonal tensions among staff, ensuring disagreements don’t spiral into performance issues or high turnover.
De-escalation techniques and NVC are especially vital during peak hours or when urgent cases strain tempers. Applying these methods maintains focus on patient priorities while diffusing emotional escalations.
Compliance alignment reinforces trust in the administration's decisions, ensuring all conflict resolution actions are both ethical and legally sound.
| Term | Definition | Application |
|---|---|---|
| Escalation Protocol | A predefined pathway for resolving conflicts that exceed standard administrative solutions. | Ensures unresolved issues don’t halt operations; e.g., a billing dispute escalated to compliance for swift resolution. |
| Root Cause Analysis (RCA) | A structured method to identify underlying factors of recurring conflicts for sustainable solutions. | Goes beyond surface issues to identify system flaws, preventing repeat conflicts. |
| Mediation | A neutral third party helps conflicting parties reach a mutually acceptable solution. | Defuses interpersonal tensions, preserves relationships, and reduces turnover. |
| De-escalation Techniques | Communication strategies to reduce tension and prevent escalation. | Vital during peak hours or stressful situations, keeping focus on patient priorities and diffusing emotional conflicts. |
| Nonviolent Communication (NVC) | Focuses on empathetic engagement and clear communication to keep discussions constructive. | Engages staff constructively, keeps discussions productive, and focuses on solutions. |
| Compliance Alignment | Ensures conflict resolution aligns with healthcare regulations (e.g., HIPAA), preventing legal issues. | Reinforces trust in decisions and ensures ethical, legal conflict resolution processes. |
Strategies for Effective Conflict Resolution
Proven Communication Tactics
In healthcare administration, effective communication is the bedrock of conflict resolution. Clear, structured communication prevents misunderstandings, ensures transparency, and streamlines issue resolution. To achieve this, medical administrators must employ targeted tactics:
Active Listening: Administrators must listen to staff concerns without interruption, demonstrating empathy and commitment to finding solutions. This approach fosters trust and reduces defensiveness.
Assertive Communication: Expressing expectations and decisions clearly, without aggression, ensures that all parties understand their roles and responsibilities.
Clarification Requests: When ambiguity arises, asking for clarification prevents the escalation of misunderstandings into disputes. This is particularly vital in complex regulatory environments.
Consistent Documentation: Keeping accurate records of discussions, decisions, and actions ensures accountability and provides a reference in case of future disputes.
These tactics, when practiced consistently, transform communication into a tool for conflict prevention rather than just resolution.
Stepwise Problem-Solving Approaches
Structured problem-solving methods are essential for resolving conflicts systematically. Effective frameworks ensure that conflicts are addressed thoroughly, minimizing the chances of recurrence:
Identify the Conflict: Recognize the core issue causing the conflict, separating facts from emotions.
Analyze Root Causes: Use Root Cause Analysis or similar frameworks to uncover underlying systemic issues.
Develop Resolution Options: Brainstorm and evaluate potential solutions, ensuring compliance with healthcare regulations and operational needs.
Implement the Solution: Roll out the agreed-upon solution with clear communication and documented steps.
Monitor and Evaluate: Follow up to ensure the resolution remains effective, adjusting protocols if new issues arise.
Incorporating these steps into daily workflows reduces reaction times and builds resilience against future conflicts. It also reinforces administrative accountability, ensuring that resolutions align with both operational goals and compliance requirements.
| Proven Communication Tactics | Stepwise Problem-Solving Approaches |
|---|---|
| Active Listening: Listening to staff concerns without interruption, demonstrating empathy and commitment to solutions. | Identify the Conflict: Recognizing the core issue of the conflict, separating facts from emotions. |
| Assertive Communication: Expressing expectations and decisions clearly, without aggression, to clarify roles and responsibilities. | Analyze Root Causes: Using RCA or similar frameworks to uncover underlying systemic issues. |
| Clarification Requests: Asking for clarification to prevent misunderstandings from escalating into disputes. | Develop Resolution Options: Brainstorming and evaluating potential solutions, ensuring regulatory and operational compliance. |
| Consistent Documentation: Keeping detailed records of discussions, decisions, and actions to ensure accountability. | Implement the Solution: Rolling out the agreed solution with clear communication and documentation. |
| Continuous Feedback: Seeking and incorporating feedback from stakeholders to refine communication strategies and strengthen team dynamics. | Monitor and Evaluate: Following up to confirm resolution effectiveness and adjusting protocols if new issues arise. |
Technology’s Role in Conflict Management
Digital Tools Supporting Conflict Tracking
Technology equips healthcare administrators with precise tools to track and manage conflicts efficiently. Integrated conflict tracking systems offer real-time visibility into issues, reducing reliance on manual reporting and enabling proactive intervention. These systems typically include:
Incident Management Platforms: Software designed to log, monitor, and analyze conflict incidents across departments. This data-driven approach supports faster resolutions and identifies trends for long-term improvement.
Workflow Automation Tools: By automating repetitive tasks, such as notifications and follow-ups, administrators can focus on resolving core issues rather than chasing paperwork.
Communication Platforms: Secure, centralized communication tools reduce miscommunication risks, ensuring stakeholders stay informed and engaged during conflict resolution processes.
Utilizing these digital solutions minimizes bottlenecks, ensures compliance with healthcare regulations, and enhances transparency throughout the conflict resolution lifecycle.
Automation in Documentation & Resolution
Automated documentation tools streamline the resolution process, reducing human error and maintaining comprehensive records. These systems offer:
Automated Record-Keeping: Digital logs capture every step of the conflict resolution process, providing auditable trails for compliance purposes.
Predefined Resolution Workflows: Templates and workflows standardize how conflicts are handled, reducing variability and promoting consistency.
Analytics and Reporting Tools: Data insights from automated systems identify recurring conflict patterns, allowing administrators to implement preventive measures.
Incorporating automation elevates administrative efficiency and ensures that even complex conflicts are resolved with regulatory compliance and minimal operational disruption.
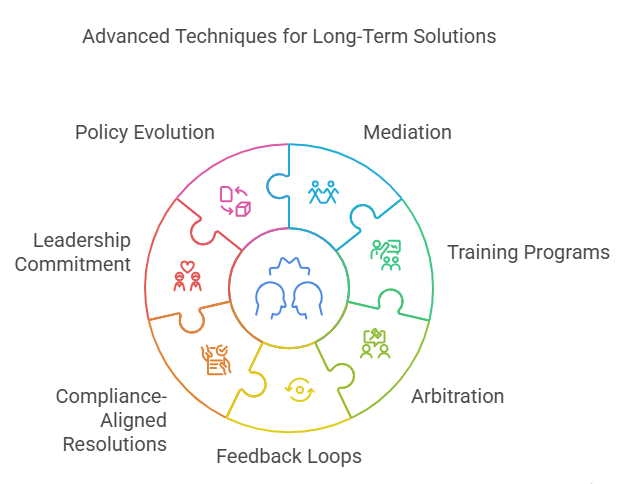
Advanced Techniques for Long-Term Solutions
Mediation and Arbitration in Healthcare Settings
Long-term conflict resolution in medical admin requires methods beyond immediate fixes. Mediation and arbitration are structured processes that offer sustainable solutions for complex or recurring conflicts:
Mediation involves a neutral facilitator who guides disputing parties toward a mutually acceptable resolution. This approach emphasizes collaboration and preserves professional relationships. In medical settings, mediation can resolve disputes over billing discrepancies, policy interpretations, or patient care disagreements.
Arbitration offers a more formal alternative where an impartial arbitrator delivers a binding decision. This method is effective for high-stakes conflicts where swift, decisive outcomes are essential. Arbitration often addresses contractual disputes with external vendors or interdepartmental issues.
Both methods reduce the strain on internal teams and legal resources, promoting efficient, compliance-aligned conflict resolution. They provide clear pathways for addressing issues that could otherwise disrupt operations and patient care delivery.
Building a Culture of Continuous Conflict Improvement
Sustainable conflict resolution isn’t about isolated incidents—it’s about fostering a culture that values proactive problem-solving and continuous improvement. Key strategies include:
Training Programs: Regular workshops and simulations ensure staff are equipped with current conflict resolution skills.
Feedback Loops: Encouraging open feedback from staff about conflict resolution processes promotes accountability and refinement.
Leadership Commitment: Visible support from senior leaders reinforces the importance of conflict resolution, ensuring it’s integrated into daily operations.
Policy Evolution: Reviewing and updating conflict management protocols keeps them aligned with evolving regulations and organizational needs.
When these strategies are embedded into the fabric of medical administration, they create an environment where conflicts are seen as opportunities for growth rather than as disruptions. This continuous improvement mindset enhances operational efficiency and builds resilience against future challenges.
How ACSMO’s Medical Scribe Certification Builds Communication Skills for High-Stakes Admin Settings
How ACMSO Certification Prepares You
The ACMSO Certification isn’t just a credential—it’s a strategic investment in mastering conflict resolution in medical administration. This program provides comprehensive training that directly applies to real-world challenges faced by healthcare administrators. Through case-based simulations and regulatory compliance modules, candidates develop the skills to navigate disputes over documentation errors, billing discrepancies, and interdepartmental resource allocation.
The curriculum emphasizes root cause analysis, proactive communication strategies, and regulatory alignment to ensure administrators are equipped to handle high-pressure situations. By focusing on structured frameworks and real-world scenarios, the certification enables graduates to identify and resolve conflicts before they escalate, maintaining operational continuity and patient safety.
Real-World Skills Gained Through the Program
Graduates of the ACMSO Certification emerge with a skill set that transforms conflict resolution from a reactive task to a proactive leadership capability:
Regulatory Navigation: Training covers HIPAA, FDA, and other healthcare compliance frameworks, ensuring all conflict resolutions are legally sound.
Advanced Communication Techniques: Participants master assertive communication, de-escalation, and mediation strategies that diffuse tensions and promote collaboration.
Process Optimization: The program’s emphasis on structured workflows and continuous improvement ensures conflicts are addressed efficiently, minimizing disruptions.
Critical Thinking and Decision-Making: Real-world case studies sharpen analytical skills, enabling participants to dissect conflicts and apply practical solutions swiftly.
These competencies position ACMSO-certified professionals as indispensable assets within medical admin teams, capable of sustaining operational integrity and enhancing patient care outcomes.
Frequently Asked Questions
-
Medical administration often faces conflicts driven by resource scarcity, workload imbalances, and communication breakdowns. Staff may experience unclear role definitions, leading to confusion about responsibilities, while time pressures can cause rushed decisions that spark disputes. Regulatory demands such as HIPAA compliance or evolving patient data protocols add layers of complexity. These challenges make it vital for healthcare administrators to implement structured conflict resolution processes, ensuring issues are swiftly addressed and operations remain compliant. When left unresolved, conflicts can escalate into systemic inefficiencies, reduced patient safety, and legal risks, ultimately eroding trust in the healthcare system. Recognizing and proactively managing these challenges is essential for operational integrity.
-
The ACMSO Certification equips healthcare administrators with practical conflict management strategies tailored for complex medical settings. It emphasizes regulatory compliance, proactive communication, and structured problem-solving frameworks such as Root Cause Analysis. Through real-world simulations and case studies, candidates learn to identify early conflict triggers, apply de-escalation techniques, and maintain operational continuity under pressure. The program focuses on bridging communication gaps, fostering collaboration, and streamlining resolution pathways. ACMSO-certified professionals not only resolve conflicts effectively but also implement preventive measures, reducing recurrence. This holistic training transforms them into strategic leaders capable of safeguarding compliance and enhancing both administrative efficiency and patient care outcomes.
-
Yes, technology plays a pivotal role in minimizing conflict incidents. Incident management platforms and digital tools offer real-time monitoring, enabling swift intervention before issues escalate. Automated workflows reduce manual errors, while secure communication systems ensure stakeholders remain aligned. Analytics capabilities identify recurring conflict patterns, allowing proactive strategy adjustments. By reducing human error and enhancing transparency, technology supports regulatory compliance and improves administrative efficiency. However, technology alone isn’t a cure-all; it must be integrated with strong leadership and clear communication protocols. When combined effectively, these tools transform conflict resolution from a reactive process to a proactive operational asset.
-
Root Cause Analysis (RCA) is essential because it identifies the underlying reasons behind recurring conflicts. Rather than addressing surface-level symptoms, RCA uncovers systemic issues such as policy gaps, training deficiencies, or misaligned workflows. By implementing corrective actions at the root level, healthcare administrators can prevent similar conflicts from arising. RCA also fosters a culture of continuous improvement, aligning conflict resolution efforts with regulatory compliance and operational goals. This approach reduces costly disruptions, enhances patient care, and reinforces staff trust in the system. Sustainable conflict resolution depends on addressing not just the immediate problem, but its origins.
-
Proactive conflict prevention starts with clear communication protocols, role definitions, and ongoing staff training. Establishing escalation pathways ensures conflicts are addressed promptly, while open feedback channels encourage staff to voice concerns early. Regular review and refinement of policies, based on regulatory updates and operational feedback, create an adaptive conflict management framework. Investing in digital tracking tools enhances transparency and ensures consistent documentation of incidents. By fostering a culture of collaboration and equipping teams with effective tools, administrators can anticipate and prevent conflicts. These proactive steps not only mitigate disruptions but also enhance overall patient safety and compliance.
-
Poor communication in medical administration magnifies misunderstandings, delays, and errors. Incomplete documentation, unclear directives, or siloed departments create an environment ripe for conflict. Misinterpretations can snowball, leading to duplicated efforts, billing discrepancies, or compliance breaches. During high-pressure situations, such as emergency intakes or critical resource allocation, lack of clarity exacerbates stress and tension. Effective communication protocols—like standardized handoff procedures, secure messaging systems, and clear escalation pathways—prevent such breakdowns. Prioritizing communication ensures that conflicts are identified and resolved early, maintaining operational integrity and supporting regulatory compliance in high-stakes medical settings.
-
Mediation and arbitration each have distinct advantages. Mediation fosters collaboration, allowing disputing parties to reach mutually agreeable solutions while preserving professional relationships. It’s particularly effective for interpersonal conflicts or billing discrepancies within healthcare teams. Arbitration, by contrast, provides a formal resolution with binding decisions, ideal for high-stakes disputes such as vendor contracts or regulatory interpretations. While mediation is often preferred for its flexibility and speed, arbitration ensures closure when parties cannot find common ground. The most effective conflict resolution strategy depends on the dispute’s complexity, stakes, and the desired outcome. Both methods complement broader conflict management frameworks in healthcare settings.
Final Thoughts
Effective conflict resolution is the cornerstone of efficient medical administration. Without it, operational disruptions, compliance breaches, and reduced patient safety become inevitable. This comprehensive approach—blending proactive communication, structured problem-solving, technology integration, and continuous improvement—forms the backbone of resilient healthcare operations. The ACMSO Certification empowers medical administrators with the practical skills and strategic frameworks needed to navigate complex disputes, ensuring issues are resolved swiftly, ethically, and in compliance with regulatory standards.
By mastering conflict resolution, certified professionals enhance workflow efficiency, safeguard compliance, and uphold the highest levels of patient care. This isn’t merely a skill—it’s a critical leadership asset that sets administrators apart. Investing in advanced training today positions organizations for a future where conflict is not a crisis but an opportunity for growth.
| How valuable do you find conflict resolution strategies in medical administration? | |
|---|---|
| Extremely valuable for operational efficiency | |
| Somewhat valuable but needs better integration | |
| Not very valuable in practice | |