Annual CMAA Salary Report: Real Data & Trends for 2026-27
In 2026 and 2027, CMAA pay is not rising because clinics suddenly became generous. It is rising in pockets because admin work is now tied to measurable outcomes like access, throughput, denials, and patient satisfaction. This report shows what the numbers say, what employers reward, and what moves actually change your paycheck.
If you want a single goal, make yourself the person who can stabilize a clinic’s day using systems from appointment scheduling efficiency, patient trust from mastering patient communication, and operational visibility from the performance metrics tools directory.
1) 2026 to 27 salary snapshot: what real data suggests and how to read it like an operator
Most “salary reports” fail because they mash different job titles together. A CMAA can sit in a clinic doing basic front desk tasks, or they can run the operational backbone of an office. Same title, wildly different value. So this report uses a simple lens: baseline market pay, then the multipliers that employers pay for.
For a baseline, two public signals matter. The first is government wage data for closely aligned roles. The BLS reports a median annual wage for medical secretaries and administrative assistants (SOC 43-6013) of $44,640 in May 2024. The second signal is job posting based pay. Indeed reports an average medical administrative assistant wage of $20.61 per hour, updated January 4, 2026, based on pay from postings.
Your 2026 to 27 reality is that employers anchor offers in that band, then adjust up when you prove you can protect revenue, reduce chaos, and keep patient flow moving. If you want to understand the wage pressure behind this, pair this report with directory of tools for improving patient flow and reducing no shows because clinics pay more when you reduce leakage.
The biggest 2026 to 27 mistake is chasing a “high salary state” without building high salary skills. State differences exist, but the consistent earners are people who can build systems. Start by mastering clean operations through efficient EMR data entry and then protect quality with patient chart audits in EMR. Those two alone separate “helpful” from “promotable.”
2) What drives CMAA pay in 2026 to 27: the levers employers actually reward
Most CMAAs try to earn more by “working harder.” Employers do not pay for effort. They pay for reduced problems. Your pay rises when you remove a pain point that costs the clinic money or reputation.
Lever one is schedule stability. If you can take a provider schedule that constantly breaks and make it predictable, you have created revenue. Build that skill using daily schedule optimization, operational guardrails from scheduling efficiency, and a patient retention layer with reducing no shows. If you can show even a small no show drop, your value becomes measurable.
Lever two is revenue protection. Clinics bleed money through preventable denials and rework. This is not a billing department problem. It starts at the front door with accuracy. Tighten inputs using efficient EMR data entry, then enforce it through chart audit mastery. When you can say, “Our registration errors dropped,” that is a raise conversation.
Lever three is patient communication under pressure. In 2026 and 2027, patients expect fast updates, clear instructions, and professional empathy. If you cannot deliver that, your phone lines become a complaint machine. Build calm scripting with telephone etiquette, clarity frameworks from patient communication, and de escalation ability from the art of empathy. This skill is invisible until it is missing, and then it destroys your day.
Lever four is tool fluency that leads to outcomes. Employers are tired of “I know the software.” They want “I can improve the metric.” That means dashboards, exports, and simple proof logs. Start with the performance metrics tools directory, then choose systems from the office management software directory, and support budget discussions using the medical office budgeting tools directory. When you speak in numbers, your pay follows.
3) Real trends for 2026 to 27: where pay rises, where it stalls, and what markets reward
Pay is not rising evenly. It rises where demand is high, where systems are failing, and where employers need operational leaders. That is why some markets hire aggressively while others cap wages.
To read the market, do not start with salary. Start with hiring pressure and complexity. If a region has rapid population growth, high provider churn, or overloaded specialties, admin roles become critical. That is why it helps to study market based guides like the New York State CMAA job market analysis, regional opportunities from Texas medical admin assistant career opportunities, and demand signals in Florida CMAA career insights. When you see where hiring is concentrated, you can target your search.
Metro areas also matter. Large systems create specialist admin tracks. Smaller clinics often pay less but can promote faster if you become the system owner. Use guides like CMAA career growth guide Los Angeles healthcare market and pressure indicators like why Chicago hospitals are hiring more CMAAs in 2025 as a pattern. The pattern is simple. Where systems are strained, operators get rewarded.
One more trend is skills based pay. Employers increasingly pay for capabilities tied to throughput and risk reduction. That includes workflow design, patient flow improvement, and compliance readiness. Build that foundation with the patient flow tools directory, lock your procedures through the policy and procedure tools directory, and keep your training sharp using the directory of CMAA certification resources. When you become the person who reduces risk and chaos, you enter a higher wage lane.
4) Negotiation in 2026 to 27: how CMAAs ask for more without sounding replaceable
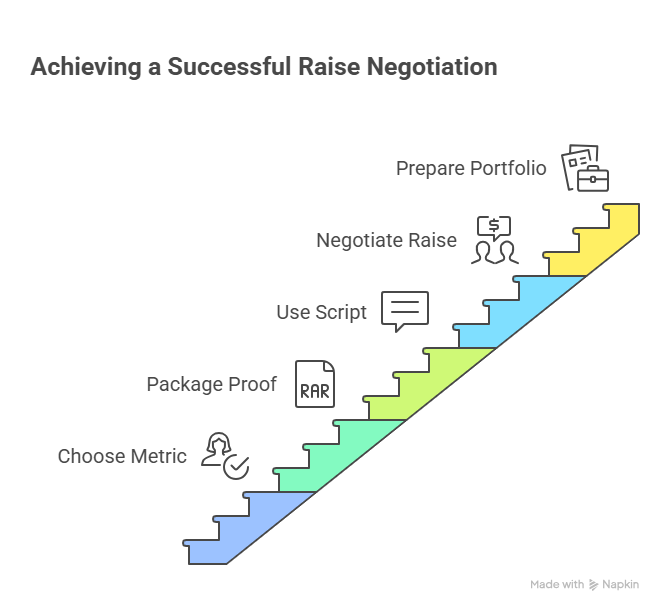
Negotiation fails when it is about feelings. It wins when it is about measurable outcomes. Your job is to walk into the conversation with proof and a plan.
Step one is choosing a metric your employer cares about. In most clinics, that is access, no shows, call abandonment, or clean first pass. If you need a ready playbook, build your plan around scheduling efficiency, reduce leakage using no show reduction, and create operational visibility with the performance metrics directory. The point is simple. Your raise is a return on investment.
Step two is packaging your proof. Bring a one page summary that includes a before number, an after number, and what you did. If you improved accuracy or reduced rework, include a QA sample log based on chart audits and your standard process from efficient EMR entry. If you reduced patient frustration, include a scripting update tied to telephone etiquette and patient communication.
Step three is using a clean script that forces the conversation onto outcomes:
“In the last 30 days, I reduced no shows from X to Y by implementing the workflow from our scheduling playbook.”
“I can expand this to cover the full clinic week if we agree on a target KPI and a review cadence.”
“Based on the value created and current market pay, I am requesting an adjustment to Z.”
If your employer refuses, you still win because you now have a portfolio for your next job. Use regional guides like California salary and job market, Florida employment trends, and New York State market analysis to target markets where systems are strained and operators are rewarded.
5) The 2026 to 27 career ladder: the fastest path to higher pay and better roles
Your best pay move is not job hopping every few months. It is moving up the value chain. The admin ladder in 2026 and 2027 is built on four levels.
Level one is reliable execution. That means accuracy, consistency, and professional communication. Anchor that using telephone etiquette, improve patient trust via the empathy guide, and tighten documentation discipline with EMR data entry. This level makes you employable. It does not make you expensive.
Level two is ownership. You own a workflow end to end. Examples include no show prevention, referral closure, or prior auth tracking. Build the system using reducing no shows and improve throughput using the patient flow tools directory. Ownership is where pay starts to separate.
Level three is measurable improvement. You run a dashboard cadence, you track results, and you coach others. Start with the metrics tools directory and combine it with standardized processes using the policy and procedure tools directory. This is where you become an operations lead candidate.
Level four is future proof fluency. Clinics are adopting automation and AI supported workflows. You do not need to be an engineer. You need to understand how automation changes inputs, routing, and QA. Study the direction in AI transforming medical administrative roles by 2030 and build readiness with emerging technologies for 2025. People who can protect quality while adopting new tools earn more.
6) FAQs
-
A realistic range depends on your role scope. For baseline market anchors, government wage data for closely aligned roles shows a May 2024 median for medical secretaries and medical admin aligned work at $44,640 annually. Job posting based data from Indeed shows about $20.61 per hour as of January 4, 2026. Your 2026 to 27 upside comes from multipliers like schedule stability, denial prevention, and KPI proof. Build those using scheduling efficiency, no show reduction, and metrics tools.
-
Owning schedule stability. If you can reduce no shows, backfill cancellations, and keep provider days predictable, you directly increase revenue. That is why it is the fastest pay lever in most clinics. Build the system using daily schedule optimization, operational structure from scheduling efficiency, and patient behavior tactics from reducing no shows. Track one KPI for 14 days, then use that proof in negotiations.
-
The best markets are not only the highest cost of living. They are markets with hiring pressure and workflow complexity. Use regional demand signals from New York State CMAA job market analysis, compare with Florida CMAA trends, and evaluate long term potential through California CMAA salary and job market. Then position yourself as an outcomes owner, not a generalist.
-
Do not argue. Reframe. Ask what outcome would justify an exception, then propose a short sprint to deliver it. For example, “If I reduce no shows by X and keep it stable for 30 days, can we revisit pay?” Run the sprint using no show reduction and track results with guidance from the metrics tools directory. If they still refuse, you leave with a portfolio that gets you paid elsewhere.
-
Training matters when it increases your operational scope. Prioritize programs that improve scheduling systems, KPI reporting, and process standardization. Use the directory of CMAA certification resources and expand skills through the interactive directory of continuing education. Combine that with measurable workflow capability using patient flow tools. Certifications support the story. Proof closes the deal.
-
AI will not erase CMAAs. It will punish inconsistent processes. In 2026 and 2027, clinics will pay more for people who can adopt automation while protecting quality, compliance, and patient experience. That includes clear routing rules, audit sampling, and standardized procedures. Use the future lens from AI transforming admin roles by 2030 and build near term readiness through emerging technologies for 2025. The pay winners will be the CMAAs who become workflow owners in an automated environment.