How to Master Patient Communication: Essential Skills for Medical Admins
Patient communication is no longer a soft skill—it’s a critical competency for medical administrative professionals. With rising patient expectations, tighter data privacy laws, and the digitization of healthcare systems, your ability to communicate clearly, accurately, and empathetically is what defines operational excellence. Miscommunication leads to costly no-shows, compliance violations, and dissatisfied patients—all of which reflect directly on the medical admin team.
Whether you’re managing front-desk interactions, coordinating post-visit follow-ups, or relaying urgent updates to care teams, your words must balance professionalism, clarity, and compassion. This guide unpacks the most vital patient communication skills, tailored for real-world clinical workflows. You’ll learn how to de-escalate tense encounters, apply HIPAA-compliant protocols in every exchange, and adopt tech tools that strengthen—not replace—your personal touch. If you’re aiming to lead, not lag, in patient satisfaction and care coordination, this is the communication blueprint you need.
Core Communication Skills in a Clinical Setting
Effective patient communication in clinical environments requires more than polite conversation—it demands structured, high-impact skills that prevent errors, enhance patient satisfaction, and keep workflows moving. Medical administrative professionals must master both interpersonal nuance and clinical accuracy, often in fast-paced or emotionally charged situations.
Verbal Clarity and Tone Management
Your tone and language must convey empathy without ambiguity. Replace vague expressions with specific instructions patients can act on. For instance, instead of “come in early,” say “arrive by 8:45 AM to complete pre-visit forms.” Avoid medical jargon unless absolutely necessary—and when it is, always follow with a plain-language explanation.
Use open-ended questions to uncover unspoken concerns.
Mirror the patient’s language level to build rapport.
Keep instructions concise and prioritize “what to do next.”
Active Listening and Reflection
Active listening is your first defense against miscommunication. It includes maintaining eye contact, affirming understanding with short feedback cues (“I see,” “Let me repeat that back”), and confirming next steps. This validates patient concerns and reduces the chance of dropped tasks or misinformation.
Restate key points to confirm accuracy.
Use reflective phrases to show understanding: “It sounds like you’re concerned about…”
Never interrupt—even during time constraints.
Nonverbal Awareness
Body language matters as much as what’s said. Patients quickly pick up on tension, disinterest, or distraction. Your posture, facial expression, and eye contact should signal attentiveness and calm. Position screens so patients don’t feel ignored while you update records.
Maintain open posture at the desk.
Nod naturally during their explanation.
Avoid multitasking while they speak.
Written Communication in Patient Materials
Every form, SMS reminder, or post-visit summary you send must meet two standards: readability and compliance. Use 6th-grade reading level where possible. Be explicit about times, locations, pre-visit requirements, and consequences for missing appointments.
Structure messages with bullet points or bolded time/date fields.
Include a contact number for questions.
For instructions: use step-by-step format with action-first language.
Cultural and Language Sensitivity
If your clinic serves multilingual or diverse populations, assume that linguistic barriers and cultural expectations affect every encounter. Prepare translated forms, work with certified interpreters (not family members), and understand how cultural norms impact eye contact, consent, or modesty.
Offer forms in the top three spoken languages in your area.
Speak directly to the patient even when using an interpreter.
Avoid assumptions—ask for preferences respectfully.
Handling Difficult Conversations with Empathy
Medical admins often stand on the front line of patient frustration—fielding complaints, billing disputes, appointment delays, or emotionally charged situations. Your ability to de-escalate these conversations while staying composed and empathetic directly affects clinic reputation, patient retention, and workflow efficiency.
Recognize the Emotional Context First
Start by identifying whether the patient is frustrated, scared, confused, or angry. Most outbursts are emotional, not personal. Respond to the emotion before the issue. This doesn’t mean agreeing—it means validating their experience:
“I understand this has been frustrating for you.”
“I hear that you're upset about the wait time.”
Acknowledgment deactivates escalation. Ignoring emotion intensifies it.
Use the “Name–Pause–Solve” Framework
Name the problem: “You’re concerned your insurance won’t cover this.”
Pause to allow the patient to respond or add context.
Solve or reframe with clarity: “Let’s go over your coverage together now.”
This structure keeps you grounded in facts while still showing empathy.
Maintain Calm Control of the Conversation
Do not match the patient’s energy. Keep your volume low and your tone slow. This regulates the emotional temperature. Use short sentences and avoid justification or blame-shifting.
Never say “That’s not my job.”
Replace with: “Let me find the right person to help you.”
Your calm sets the ceiling for how intense the interaction becomes.
Know When to Escalate Strategically
You are not obligated to resolve every issue alone. If the conversation veers into aggression, personal insults, or complex clinical questions, involve the appropriate supervisor or provider without delay.
Set boundaries respectfully: “I’m here to help, but I’ll need to bring in my supervisor to assist from here.”
Document the interaction in the patient record if needed.
Use Aftercare to Rebuild Trust
If the conversation ends neutrally or positively, follow up with action. This could be a courtesy call confirming the solution, a follow-up email, or ensuring the provider addresses the issue in the next visit. Patients remember resolution more than the conflict itself.
Example: “I’ve noted this for your physician to review with you directly at your visit next Tuesday.”
| Strategy | Implementation | Benefit |
|---|---|---|
| Acknowledge Emotion | Actively listen and validate the patient’s frustration, anxiety, or confusion before attempting to resolve the issue. Use reflective phrases like “I understand this has been upsetting for you.” | De-escalates tension early by showing empathy before jumping to solutions. |
| Stay Calm and Controlled | Speak in a low, steady voice. Keep your tone neutral and avoid matching the patient’s emotional intensity, even if they become upset or aggressive. | Prevents emotional escalation and maintains professional boundaries. |
| Use “Name–Pause–Solve” | State the patient’s concern clearly, pause to let them respond or clarify, then propose a solution using calm and clear language. | Creates a calm, structured interaction that patients can easily follow and respond to. |
| Escalate When Needed | Identify when a situation exceeds your scope—such as billing disputes, safety concerns, or clinical confusion—and refer to the appropriate supervisor or department quickly. | Protects boundaries, ensures resolution by appropriate authority, and prevents staff burnout. |
| Follow Up | After the issue is resolved, send a confirmation email, call, or note in the EHR that acknowledges the resolution and invites further feedback. | Rebuilds patient trust, shows accountability, and closes the loop effectively. |
Using Technology to Enhance Patient Interaction
Tech doesn’t replace the human element—it amplifies patient connection when used with intention. Medical administrative staff can harness digital tools to streamline communication, personalize engagement, and reinforce clarity before, during, and after the visit.
Automating the Right Touchpoints
Automated systems save time, but only when applied to non-sensitive, high-frequency tasks. Appointment confirmations, reminders, intake forms, and post-visit feedback surveys are perfect use cases.
Use SMS/email reminders with precise time, location, and required documents.
Offer one-click rescheduling via patient portals.
Avoid automating anything involving complaints, billing disputes, or clinical guidance.
Patients expect quick, actionable notifications, not generic bulk messages.
Real-Time Messaging for Clarity
Secure messaging platforms (often integrated into EHRs or patient portals) enable direct, asynchronous communication between staff and patients. Use this for scheduling clarification, insurance queries, and follow-up logistics—not for medical advice.
Template messages can reduce typing time while maintaining tone.
Always identify yourself clearly in the message.
Set boundaries on response times (e.g., “Replies may take up to 24 hours”).
This builds reliability without overstretching your team.
Patient Portals: Underused, High-Value Tools
Most patients don’t explore portal features unless they’re encouraged to. As an admin, it’s your role to guide them toward tools that improve transparency and self-service:
Show patients how to view lab results, update insurance, or message providers.
Use printouts or screenshare demos during check-in.
Emphasize privacy and HIPAA compliance for hesitant users.
Portals reduce phone call volume and allow patients to engage with care on their terms.
Video Call Etiquette for Virtual Front Desks
As telehealth expands, so does the role of virtual admin interaction. You might now greet patients on video, verify documents, or help troubleshoot tech issues before a provider joins. This requires:
Clear camera framing and a quiet environment.
Eye contact via camera, not screen.
Short scripts for greeting, verifying, and handing off the call.
Professionalism here directly shapes how seriously patients view the entire visit.
Analytics-Driven Personalization
Modern systems allow you to track missed appointments, communication preferences, and patient satisfaction feedback. Use this data to refine how, when, and how often you reach out.
Flag patients who prefer calls over emails.
Reduce reminders for those who consistently confirm early.
Review survey keywords to identify recurring friction points.
The goal isn’t just efficiency—it’s measurable engagement and better retention.
| Tool/Platform | Best Use | Admin Advantage |
|---|---|---|
| Automated Reminders | Used for sending appointment confirmations, form completion alerts, and visit follow-up reminders through SMS or email. | Significantly reduces no-show rates, improves patient preparedness, and saves staff time on repetitive calls. |
| Secure Messaging | Ideal for clarifying appointment details, insurance queries, and documentation issues in a HIPAA-compliant way. | Keeps patient communication centralized, secure, and trackable without interrupting the office workflow. |
| Patient Portals | Allows patients to view lab results, message providers, update contact info, and manage appointments on their own schedule. | Transfers routine administrative tasks to the patient side, reducing call volume and empowering engagement. |
| EHR Flags/Tasks | Used to tag patient records with communication preferences, follow-up needs, or custom alerts for front desk awareness. | Ensures that personalized and timely actions are taken, improving continuity and reducing oversights. |
| Video Front Desk | Supports remote patient check-in, identity verification, tech onboarding, and smooth transitions to providers in telehealth. | Creates a polished, professional experience for virtual visits, improving patient confidence in digital care delivery. |
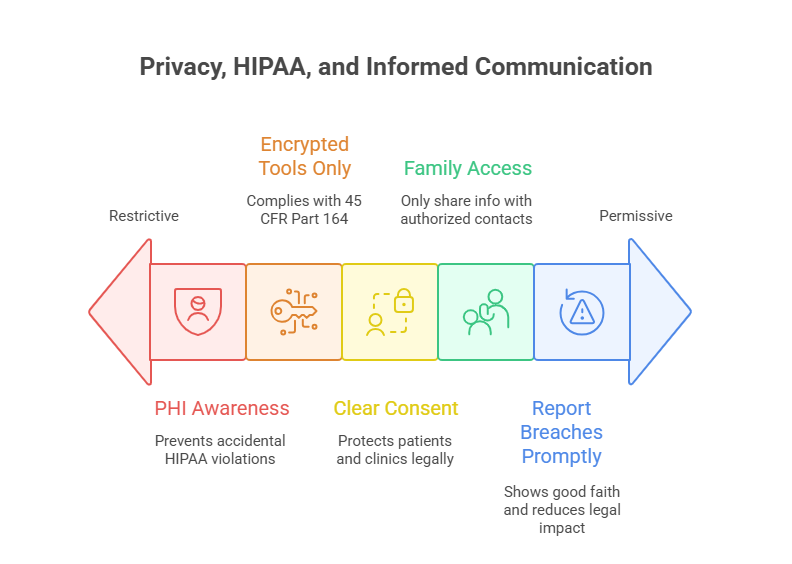
Privacy, HIPAA, and Informed Communication
Every interaction with a patient—spoken, written, or digital—must comply with HIPAA regulations and ethical transparency standards. But beyond compliance, the most effective medical admins use proactive communication habits that build trust while reducing legal risk.
Understand What Constitutes Protected Health Information (PHI)
PHI includes anything that can identify a patient—names, addresses, appointment times, diagnoses, billing info. Even casual hallway comments can violate HIPAA if overheard. Always:
Avoid discussing patient cases in shared spaces.
Lock screens when stepping away from workstations.
Never confirm or deny treatment details to unauthorized parties.
Privacy violations often happen unintentionally—through casual conversation, not malice.
Secure Channels Only—No Exceptions
Texting a friend is not the same as texting a patient. You must use encrypted, HIPAA-compliant systems for all electronic patient communication—even if it’s “just a quick reminder.”
Never use personal phones or email for patient data.
Ensure any patient-facing platform meets 45 CFR Part 164 security standards.
Educate new staff on approved communication channels.
Consistency in these rules is your first line of defense during audits.
Clarify Consent for Each Touchpoint
Informed communication isn’t just a clinical responsibility. Admins must explain what data will be used, how it’s stored, and who can access it—especially with intake forms, third-party billing services, or external referrals.
Use plain-language consent explanations: “This allows us to share test results with your specialist.”
Confirm preferred contact methods: call, SMS, portal?
Document all consent decisions in the record.
Verbal consent is not enough—you must verify, clarify, and log it.
Handling Family Members and Caregivers
Just because someone is a spouse or parent doesn’t mean they’re authorized to access a patient’s information. When dealing with minors, elderly patients, or those with cognitive issues, request:
A signed release or power of attorney.
Verification documents, when applicable.
Consent from the patient if they are capable.
Never guess based on relationship—only act on documented authorization.
Breach Response Starts with Admin Awareness
If you suspect a data breach—email sent to wrong address, overheard diagnosis, misplaced form—immediately notify your privacy officer or supervisor. Swift response mitigates legal exposure and shows good-faith compliance.
Log the incident and who was notified.
Never attempt to cover up or delay reporting.
Follow up to confirm mitigation actions were taken.
Patients trust your clinic with their most sensitive data. That trust is only preserved through airtight, proactive protocols.
Building Long-Term Patient Trust
Trust isn’t built through a single positive encounter—it’s earned through consistent, respectful, and transparent communication across the entire patient journey. For medical administrative professionals, this means turning routine tasks into micro-moments of reliability that shape how patients perceive the entire clinical experience.
Start Strong: First Impressions at Check-In
A patient’s trust-building experience starts at the front desk, not the exam room. This is where tone, pace, and attention to detail matter most.
Greet each patient by name and confirm appointment details confidently.
Offer assistance without prompting—especially for forms or tech issues.
Make eye contact and avoid multitasking when they're speaking.
The front desk sets the tone: are you rushed and reactive, or prepared and attentive?
Follow-Through Builds More Trust Than Promises
It’s not what you say—it’s whether you follow through. If you say you’ll call with results, call. If there’s a delay in paperwork, update them proactively. Patients remember whether you did what you said more than they remember what you said.
Use task lists or EHR flags to remind yourself of promised actions.
Confirm completion verbally or via secure message: “Your form has been sent.”
Close the loop—never assume silence means satisfaction.
Own Mistakes and Recover Fast
When something goes wrong—an overbooked slot, insurance mismatch, missing referral—acknowledge the error immediately. Defensive responses kill trust. Clear ownership plus a swift fix earns respect.
“That’s our error, and I’ll fix it now.”
“Thank you for catching that—I’m updating it in real time.”
People don’t expect perfection. They expect responsibility.
Personalization Without Breaching Boundaries
Small personal touches make patients feel seen—but only when done respectfully. Use notes in the system to track communication preferences or relevant concerns they’ve voiced.
Remember a preferred name or title (“Ms. Patel prefers text reminders”).
Acknowledge major health milestones or challenges, with discretion.
Offer consistency in how they’re greeted and engaged.
Personalization should always feel natural, never scripted.
Train for Emotional Intelligence
Admins often encounter patients at their most vulnerable—post-diagnosis, post-op, or amid insurance confusion. Emotional intelligence (EQ) allows you to navigate these moments with tact.
Recognize nonverbal cues of anxiety or confusion.
De-escalate by slowing your speech and softening tone.
Reflect the patient’s emotional state back with validating phrases.
When patients feel understood, they associate that feeling with your facility.
ACMSO’s Certification for Medical Admin Professionals
If you're serious about mastering patient communication and elevating your clinical career, the ACMSO Medical Administrative Certification offers the structured, industry-backed training you need. Designed to reflect real-world healthcare demands, this program blends core admin functions with advanced patient engagement, HIPAA compliance, and digital communication strategy—turning you into an indispensable asset at any clinic or hospital.
What Sets ACMSO’s Program Apart?
Unlike general admin courses, ACMSO’s certification is built around the core realities of patient-facing clinical environments. You won’t waste time on theory or generic office tasks. Every module connects to measurable outcomes: reduced patient complaints, better scheduling accuracy, faster intake turnaround, and stronger compliance.
HIPAA-Compliant Communication: Learn exactly how to handle PHI in speech, forms, and tech.
De-Escalation Frameworks: Get practical techniques for resolving conflict without authority over clinical decisions.
Tech Stack Training: Gain hands-on knowledge of EHR systems, secure messaging platforms, and patient portals.
The certification turns routine duties into strategic functions that directly impact patient satisfaction and clinic operations.
Career Impact and ROI
Graduates of the ACMSO Medical Administrative Certification often report faster job placements, higher pay bands, and greater upward mobility. Clinics and hospitals are actively seeking staff who understand not just what to do, but how to communicate it with clarity and care.
Adds credibility to your resume in a competitive hiring market.
Prepares you for team lead, trainer, or patient liaison roles.
Boosts confidence when dealing with patients, providers, and insurers.
You’re not just learning to answer phones—you’re learning how to manage information, emotion, and compliance simultaneously.
How to Enroll
The course is 100% online and self-paced, designed for working professionals. You can complete it alongside your current role, with full access to instructors, downloadable templates, and exam prep tools.
Whether you're just entering the field or already working at a front desk, this is your opportunity to formalize your skills, earn recognition, and become the admin every clinic wants to keep.
Frequently Asked Questions
-
The most essential skills include active listening, clear verbal delivery, and empathy under pressure. Admins must also master nonverbal communication cues like tone, posture, and eye contact. Being able to simplify complex processes—like insurance verification or consent forms—into patient-friendly language is key. Strong medical admins use scripts not to sound robotic but to stay compliant and consistent. Emotional intelligence is equally critical; it helps manage frustrated patients without escalating the situation. Finally, reliability—doing what you say you’ll do—cements patient trust. Communication isn’t just about talking—it’s about making patients feel heard, safe, and confident in your care coordination.
-
Start by recognizing that most difficult interactions are rooted in fear, confusion, or frustration—not disrespect. Use a calm tone and avoid defensive language. Validate the patient's concern before addressing the logistics: “I hear this has been frustrating. Let’s take it one step at a time.” The “Name–Pause–Solve” framework helps: name the issue, pause for their input, and propose a solution. Always maintain control over your energy level and voice modulation. If a situation goes beyond your role, escalate with professionalism: “I’m going to bring in my supervisor so we can support you better.” Follow up to rebuild trust.
-
HIPAA ensures patient confidentiality and data security, protecting sensitive information across all forms of communication—verbal, written, and digital. Violating HIPAA, even unintentionally, can result in fines, legal action, and reputational damage to your clinic. For admins, HIPAA isn’t just policy—it’s embedded in how you verify identity, relay lab results, handle calls, or email appointment details. Using approved systems, obtaining clear consent, and avoiding casual disclosures are non-negotiable. Even saying “I saw your test results” in a hallway can breach compliance. HIPAA matters because trust is impossible without privacy, and trust is the core of healthcare communication.
-
Technology, when used strategically, boosts clarity, access, and patient engagement. Automated reminders reduce no-shows. Patient portals allow patients to view lab results, message providers, and manage their care proactively. Secure messaging platforms help admins clarify logistics without playing phone tag. EHR flags help track promised callbacks or special patient notes. Analytics can identify communication bottlenecks—like frequently missed instructions or patients who prefer texts over emails. However, technology should enhance—not replace—human interaction. Patients still expect empathy, not just efficiency. When tech and tone work together, communication becomes faster, smarter, and more patient-centered.
-
Personalization starts with acknowledging patient preferences—names, pronouns, language choices, and communication methods. Admins should use EHR notes to remember if someone prefers text over calls or needs a language interpreter. Referencing a past visit or health goal builds familiarity. However, avoid overstepping boundaries: don’t comment on appearance, make assumptions about relationships, or discuss personal matters. Always stay neutral and professional. The goal is to make patients feel seen and supported—not scrutinized. Effective personalization is discreet, relevant, and tied directly to the care experience, not personal opinions or unsolicited commentary.
-
Emotional intelligence enables you to read patient moods, adapt communication styles, and prevent conflict before it escalates. High EQ admins notice when a patient is anxious, even if they’re quiet, and adjust tone accordingly. They listen with presence, validate emotions without becoming overwhelmed, and stay solution-focused even under pressure. EQ also helps in team dynamics—collaborating with providers, relaying urgent issues clearly, and avoiding blame language. It’s what separates a task-completer from a true coordinator. In a high-stakes, high-emotion field like healthcare, emotional intelligence makes you a steadying force in moments of uncertainty.
-
The ACMSO Medical Scribe Certification equips you with real-world patient communication tools, HIPAA protocols, digital fluency, and de-escalation strategies—all packaged in a self-paced, career-focused curriculum. Unlike generic admin courses, it’s tailored for clinical settings, with modules covering EHR usage, consent processes, and cross-cultural communication. Graduates gain a competitive edge in hiring and often step into leadership roles faster. The certification also signals to employers that you’re not just clerical—you’re a patient-facing professional who understands compliance, compassion, and coordination. It’s ideal for those who want to move beyond front-desk work and into clinic operations leadership.
The Take Away
Mastering patient communication isn’t an optional soft skill—it’s the operational backbone of every medical office. From the front desk to post-visit follow-ups, the way you speak, write, listen, and respond shapes patient trust, compliance outcomes, and clinic efficiency. With rising expectations and tighter regulations, clinics need medical admins who can navigate emotion, enforce privacy, and use tech with precision. Whether you're managing intake or resolving complex concerns, each word you choose carries weight. Training isn’t just helpful—it’s essential. The ACMSO Medical Admin Certification gives you the tools to lead those conversations with confidence, clarity, and care. This isn’t about checking boxes—it’s about becoming the voice patients trust when the stakes are high.
Which area of patient communication do you find most challenging?