Directory of Tools for Improving Patient Flow in Medical Offices
Managing patient flow isn’t just a logistics issue — it’s a profitability, compliance, and care quality imperative. Every minute lost in scheduling bottlenecks, documentation delays, or waiting room backups compounds into dissatisfied patients and mounting overhead costs. In today’s healthcare market, streamlining flow isn’t optional. It’s the frontline of operational efficiency, especially as practices face shrinking reimbursements, rising staffing costs, and heightened patient expectations. A single improvement in throughput time can increase revenue per provider by over 15%, while also reducing staff burnout and patient attrition.
This guide breaks down real-world digital tools that actively improve patient throughput — not generic systems or outdated tactics. Whether you're running a small dermatology clinic or a multi-specialty group practice, these software categories can help eliminate friction, reduce no-shows, enhance compliance, and create measurable gains in visit-to-reimbursement time. From EHR-integrated scheduling to smart KPI dashboards and certified scribe support, we’ll cover tools that aren’t just nice-to-have — they’re mission-critical.
What Patient Flow Means and Why It Matters
Patient flow is the movement of individuals through a medical office, from arrival to discharge. It includes appointment scheduling, intake, rooming, treatment, documentation, billing, and follow-up. Optimizing this flow isn’t about speed alone — it’s about reducing bottlenecks, minimizing idle time, and ensuring every patient interaction is clinically efficient and operationally lean.
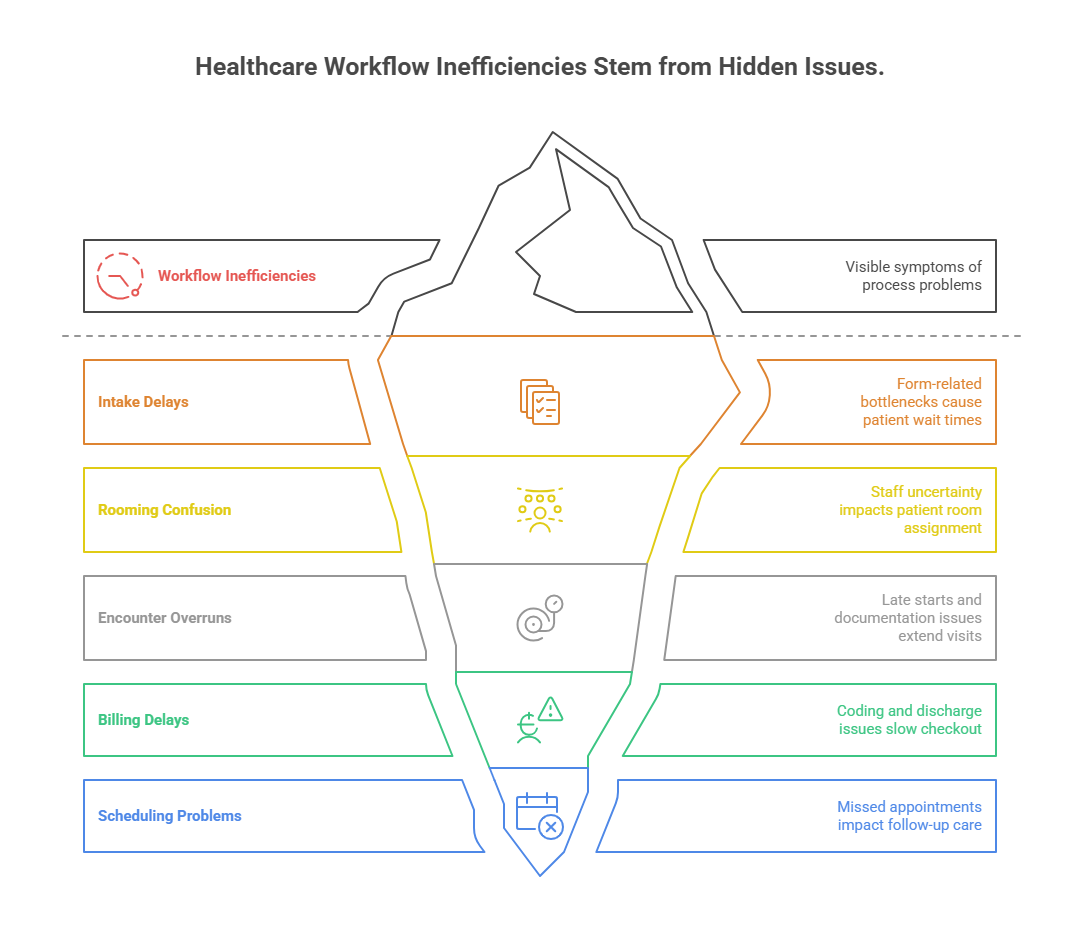
Hidden Costs of Poor Flow
Poor patient flow quietly erodes performance. Delays in room turnover, disjointed communication, or outdated scheduling tools create backlogs that inflate staffing costs, frustrate patients, and decrease daily visit volumes. A 2024 MGMA survey showed practices with top-quartile flow metrics earned 21% more per FTE physician compared to their peers.
When providers are waiting on exam rooms, or medical assistants are idle due to uncoordinated tasking, you're burning payroll without care delivery. Worse, patients stuck in waiting rooms often leave without treatment — or never return.
Patient Experience and Retention
In a market where patients have choices, flow equals reputation. A fast, seamless visit boosts online reviews, retention, and word-of-mouth referrals. Poor flow leads to “doctor shopping,” lower star ratings, and poor Press Ganey scores — all of which directly affect payer negotiations and new patient growth.
Regulatory and Reimbursement Implications
CMS and private insurers are increasingly tying value-based payments to operational benchmarks like wait times and throughput. Practices with consistently poor flow data may face reduced reimbursements, fewer referrals, and increased audit scrutiny. Tools that optimize flow are not just efficiency drivers — they’re compliance safeguards.
EHR and Scheduling Solutions for Flow Optimization
The backbone of efficient patient flow is a tightly integrated Electronic Health Record (EHR) and scheduling system. When these tools are fragmented, delays become routine. But when configured correctly, they become the central nervous system for fast, coordinated care delivery.
What to Look for in Flow-Optimized EHRs
EHRs that improve patient flow offer more than charting — they enable real-time visibility across the entire visit cycle:
Smart appointment slotting: Auto-fill based on appointment type, staff availability, and room capacity.
Pre-visit data collection: Mobile check-ins and symptom questionnaires reduce intake delays.
Status tracking: Flags showing patient location (waiting, roomed, discharged) keep all staff aligned.
Solutions like athenahealth, DrChrono, and Epic are known for their workflow configurability and built-in flow analytics.
Advanced Scheduling Features That Reduce Waste
Poor scheduling is the single largest upstream bottleneck. Practices lose tens of thousands annually due to unfilled slots, double bookings, or high no-show rates. Tools like:
Predictive scheduling algorithms adjust templates based on no-show trends.
Waitlist automation fills last-minute cancellations to protect revenue.
Integrated telehealth slots offer virtual flexibility during high in-office congestion.
These features ensure that provider time is always matched to demand — not wasted.
ROI from Smart Scheduling
Practices that implement smart EHR scheduling reduce average cycle times by 15–25% within the first quarter, according to AMA benchmarking data. That translates to 3–5 extra visits per provider, per day, boosting both care access and bottom line. And with audit-ready logs and automated time-stamping, billing integrity improves too.
Real-Time Tracking Tools and Their Benefits
Real-time tracking systems are no longer reserved for hospitals — they’re now essential in outpatient clinics, urgent care centers, and multispecialty medical offices. These tools allow you to track patient location, staff availability, and room utilization minute-by-minute, closing the feedback loop on delays before they spiral.
Key Capabilities of Real-Time Location Systems (RTLS)
RTLS uses RFID tags, Bluetooth beacons, or Wi-Fi-enabled badges to monitor patient and equipment movement through the clinic. Leading systems such as Midmark RTLS and Sonitor provide:
Live patient location data: See who is in the waiting room, being triaged, or ready for checkout.
Staff task tracking: Know which MA or nurse is with which patient and when.
Room turnover alerts: Automate notifications when exam rooms are cleaned and ready.
This kind of visibility eliminates time-wasting “Where is the patient?” or “Has the doctor seen them yet?” guesswork.
Quantifiable Operational Gains
According to a 2024 case study by the Advisory Board, clinics using RTLS saw:
A 35% reduction in patient wait times
A 22% improvement in exam room turnover
A 17% increase in daily patient throughput
Even more critically, these tools provide audit-ready logs that support compliance, staff accountability, and continuous improvement.
Enhancing the Patient Experience
Patients appreciate transparency. Tools that enable text alerts for wait updates, mobile check-in confirmations, or touchscreen kiosks for intake can dramatically reduce perceived wait times and increase satisfaction. A smoother flow not only improves care — it enhances loyalty and boosts referral retention.
| Tracking Feature | Operational Impact |
|---|---|
| Patient Location Monitoring | Provides real-time visibility of each patient's position in the care journey, allowing staff to proactively manage rooming and reduce gaps between clinical touchpoints. |
| Room Turnover Alerts | Notifies cleaning staff and clinical teams instantly when a room is vacated and ready, accelerating exam room availability and maximizing usage across the day. |
| Staff Task Visibility | Displays which team members are assigned to which patients, reducing confusion, improving team handoffs, and ensuring every patient receives timely care from the right provider. |
| Kiosk Status Updates | Offers patients live feedback on check-in status, queue placement, and estimated wait times, improving transparency and decreasing perceived delays and frustration. |
| Audit Trail Logs | Captures time-stamped movement and actions across the patient journey for compliance, staff accountability, and process improvement audits. |
Billing and Documentation Software Impact
Billing and documentation systems are often viewed as backend functions, but in reality, they sit at the core of patient flow efficiency. When your documentation tools are clunky or billing workflows rely on manual processes, the result is delayed chart closure, overworked staff, and slowed patient discharge — all of which jam the pipeline.
The Hidden Flow Bottlenecks in Documentation
Even with advanced EHRs, documentation delays persist. Why?
Clinician note fatigue: Manual data entry leads to late charting and backlogs.
Unstructured data input: Inconsistent templates create review bottlenecks during coding.
Delayed charge capture: Slows billing, AR, and follow-up appointment scheduling.
A 2025 MGMA study found that clinics with outdated documentation systems lost an average of $78,000 per provider annually due to inefficiencies in flow-related billing delays.
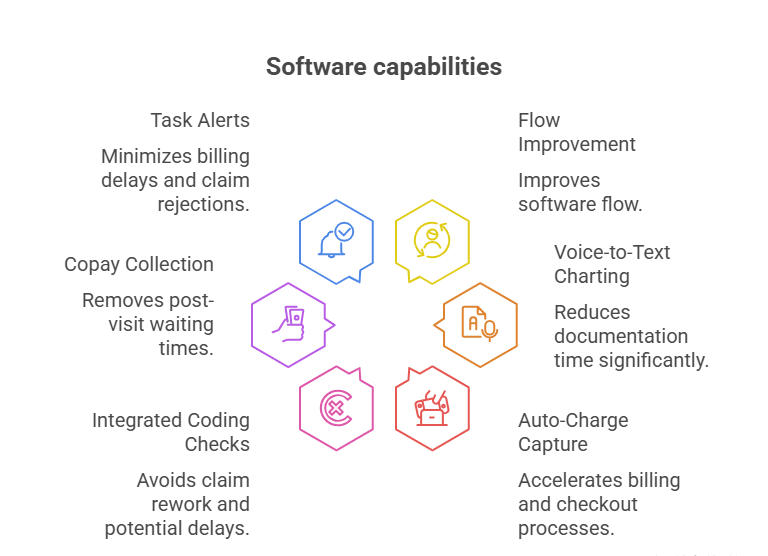
Automation That Frees the Pipeline
Smart documentation tools like PhraseExpander, Nuance Dragon Medical One, and SOAPware use:
Voice recognition and macros to streamline note creation.
AI-assisted templates that auto-fill based on visit type and ICD/CPT selection.
Integrated charge capture that syncs with billing in real time.
This allows providers to complete documentation at point-of-care, not at the end of the day — improving chart closure rates and keeping visits moving.
Billing Software’s Direct Flow Contribution
Revenue cycle tools like Kareo, AdvancedMD, and PracticeSuite support flow by:
Eliminating paper superbills and reducing errors in claim creation.
Automating eligibility checks and copay collection before or during check-in.
Flagging incomplete documentation to prevent downstream denial delays.
When patients aren’t held at checkout waiting on copay processing or discharge instructions, cycle time drops and satisfaction rises. Simultaneously, your billing team gets cleaner claims, fewer rejections, and better cash flow — with no extra admin labor.
KPI Dashboards and Custom Workflow Tools
You can’t improve what you don’t measure. KPI dashboards and workflow tools give medical practices visibility into exactly where inefficiencies lie — and how to fix them. Without them, you're flying blind, relying on anecdotal complaints rather than quantifiable data to drive decisions.
What a Good KPI Dashboard Should Track
Effective dashboards go beyond revenue reports. They track flow-critical metrics in real time, including:
Patient cycle time: From check-in to checkout
Room utilization rate: Time spent occupied vs. idle
Provider throughput: Patients seen per provider per hour
No-show and cancellation rates
Front desk check-in time and call response delay
Systems like Tableau for Healthcare, Power BI with EMR integrations, or built-in analytics in tools like NextGen provide actionable, drill-down data that turns insights into interventions.
Custom Workflow Builders: Beyond Generic EHR Templates
Flow optimization demands customization. Tools like:
Pipefy and Kissflow allow drag-and-drop task routing
Jotform Approvals streamline staff handoffs
Zapier integrations automate repetitive admin steps
These allow you to build workflows that reflect how your clinic operates — not generic hospital logic. For example, you can design a task flow where front desk alerts the MA when intake is complete, and the MA triggers a text when the room is ready. Zero confusion. Zero lag.
From Visibility to Accountability
With dashboards, data is no longer buried in backend reports. Frontline teams can see their metrics daily — enabling data-driven standups, performance reviews, and instant bottleneck detection. Clinics that implement daily or weekly KPI reviews have reported up to 28% improvement in cycle time within two months, according to a 2025 MGMA analytics survey.
| Metric or Tool | Flow Optimization Use |
|---|---|
| Cycle Time Tracking | Measures the total time a patient spends from check-in to checkout, allowing clinics to isolate specific stages (intake, rooming, discharge) that cause delays and require targeted workflow changes. |
| Room Utilization Rate | Analyzes how frequently and efficiently exam rooms are used, helping identify underused spaces or scheduling gaps that contribute to long wait times and reduce patient throughput. |
| Custom Task Routing | Automates the assignment of admin and clinical tasks based on role, availability, or status (e.g., MA notified when intake is complete), which reduces handoff errors and speeds up patient transitions. |
| Real-Time Dashboards | Provides instant visibility into key performance indicators like no-show rates, wait times, and staff productivity, enabling on-the-fly adjustments and real-time troubleshooting. |
| Workflow Builders (e.g. Pipefy) | Allow clinics to design drag-and-drop workflows customized to their operations, replacing generic EHR pathways with real-world process logic that matches actual staff behavior and resource constraints. |
Get Certified in Medical Scribing or Admin via ACMSO
Tools and software can only go so far if your team lacks the workflow literacy and documentation skills to use them efficiently. That’s where upskilling becomes non-negotiable. The ACMSO Medical Scribe and Admin Certification bridges that gap by training professionals in patient flow mechanics, EHR command, billing prep, and documentation speed — all within a clinical compliance framework.
Why Certification Matters for Patient Flow
Hiring a certified scribe or admin doesn't just reduce provider documentation burden — it directly accelerates the entire visit lifecycle. Trained professionals from ACMSO:
Capture notes in real-time, freeing the physician to focus on care
Understand the logic behind appointment templates and flow blocks
Flag billing red flags before they stall downstream reimbursement
Know when to escalate delays to preserve throughput
Whether you're building a lean private practice or scaling a multi-site clinic, this certification gives your team operational fluency, not just admin training.
What You’ll Learn in the ACMSO Program
The certification includes:
200+ lessons across EHR usage, scheduling logic, intake-to-billing flow, and compliance
Real-world case simulations that mirror daily practice bottlenecks
CPT, ICD, and HCPCS fundamentals for faster documentation routing
Workflow optimization labs with mock dashboards and cycle-time calculators
Graduates don’t just learn the “what” — they’re trained to implement the “how” that directly impacts patient flow.
Start Building a Flow-Smart Team
The difference between a front desk that fumbles and one that runs like clockwork often comes down to training. Enroll in the ACMSO Medical Scribe and Admin Certification to create a team that’s built for speed, accuracy, and daily flow wins — from intake to billing close.
Frequently Asked Questions
-
The single most impactful software for small clinics is an integrated EHR and smart scheduling system. These platforms streamline check-in, auto-assign rooms, and reduce idle time through predictive scheduling. Tools like athenahealth or DrChrono offer built-in flow metrics and can integrate with billing and eligibility systems. Clinics using EHRs with embedded scheduling features report up to 30% lower no-show rates and 20% faster room turnover. For small teams, this can mean seeing 4–6 more patients per day without adding staff or space. When paired with mobile intake and documentation tools, these platforms can optimize the entire care journey from front desk to billing.
-
RTLS works by tracking the location of patients, staff, and equipment in real time, eliminating delays caused by miscommunication or unclear room status. Systems like Midmark RTLS send instant alerts when a patient is ready or a room is cleaned, allowing for faster transitions between care stages. This leads to smoother handoffs, less idle staff time, and improved room utilization. Clinics using RTLS report up to 35% reduction in patient wait time and significantly higher satisfaction scores. By removing uncertainty from daily operations, these systems enhance both productivity and patient experience.
-
Certified medical scribes do far more than document — they actively unlock bottlenecks across the entire visit. By handling live charting during encounters, they eliminate the need for physicians to back-chart or delay next appointments. This improves provider throughput, shortens cycle time, and allows faster room re-entry. Trained scribes from programs like ACMSO are taught to integrate with billing workflows, alert teams of incomplete fields, and track flow metrics. Studies show scribes increase provider efficiency by 15–20%, translating into more visits per day and higher revenue without compromising care quality.
-
Key flow metrics include: average patient cycle time, room utilization rate, patients-per-hour per provider, no-show rate, check-in time, and discharge-to-billing lag. These indicators reveal exactly where your bottlenecks are. Tools like Power BI, Tableau, or native EHR dashboards can help visualize these in real time. Top-performing clinics review these metrics weekly in 10-minute team standups. When tracked consistently, cycle times improve by 20–30% within a quarter, and patient satisfaction scores increase. Tracking without action is useless, though — dashboards only work when paired with workflow corrections and accountable staff ownership.
-
Digital intake forms and kiosks reduce front-desk workload and cut waiting room congestion. When patients complete forms via mobile or kiosk before the appointment, MAs and providers access structured data instantly — speeding up triage and exam start time. Kiosks also support real-time insurance verification, payment collection, and consent capture, all without staff intervention. Clinics using kiosks report 10–20% cycle time reduction and lower data entry errors. They’re especially valuable during peak hours, allowing staff to focus on higher-value tasks while improving compliance and documentation integrity.
-
The ROI is both financial and operational. Practices adopting flow-optimized tools report:
3–5 additional visits per provider per day
Up to 25% higher revenue per FTE provider
Improved patient satisfaction scores (often leading to more referrals)
Fewer billing errors and faster collections
For example, implementing a smart EHR and real-time tracking system may cost $10K–$20K upfront, but can yield 6-figure revenue gains within 12–18 months through higher throughput and fewer missed opportunities. The non-monetary return — better staff morale, less burnout, higher patient retention — is just as critical.
-
Yes. Multi-site and specialty practices benefit from tools that offer role-based access, centralized analytics, and specialty-specific templates. Platforms like Epic, eClinicalWorks, and AdvancedMD support workflows tailored for cardiology, orthopedics, dermatology, etc. Specialty templates reduce charting time and improve accuracy. Centralized dashboards allow leadership to compare performance across locations and standardize best practices. Integration with specialty imaging or lab tools also improves flow. For example, in dermatology, photo documentation apps integrated into the EHR can reduce redundant data entry and accelerate post-visit documentation.
Final Thoughts
Improving patient flow isn’t about chasing perfection — it’s about removing friction, accelerating care, and increasing revenue without adding staff. Whether you’re investing in real-time tracking, automating intake, or training admin staff through certification programs like ACMSO, every step contributes to measurable gains in efficiency and patient satisfaction.
High-performing medical offices aren’t guessing — they’re using data, tools, and training to turn patient movement into a competitive advantage. If your practice still relies on manual processes or siloed systems, the time to modernize is now. Start with one bottleneck. Choose one tool. Track one KPI. Because every minute saved in patient flow adds margin, quality, and momentum — and that’s how modern clinics win.
Poll: Which tool has had the biggest impact on improving patient flow in your clinic?