Best Tools for Medical Office Performance Metrics (Interactive Directory)
Modern medical offices operate in a high-stakes, data-driven environment. With thin margins and rising patient expectations, clinics that lack performance visibility fall behind—fast. Tracking metrics isn’t about vanity numbers. It’s about real-time decision-making, faster reimbursements, reduced patient churn, and compliance peace of mind. But with hundreds of KPIs and dozens of software tools available, most practices either track the wrong metrics or use tools that don’t scale. The result? Missed revenue, burnt-out staff, and underperforming systems.
The solution lies in precision tooling paired with actionable metrics. From real-time dashboards and EHR-integrated reports to customized analytics via Excel models and BI platforms, the right toolset empowers practice managers to reduce AR days, spot patient experience gaps, and forecast financial risks. This interactive guide is not just a list—it’s a clinic-optimized directory designed to help you find the tools that align with your clinic size, budget, and performance goals. Whether you run a solo practice or manage a multi-location network, every tool we cover is selected for one reason only: measurable performance improvement.
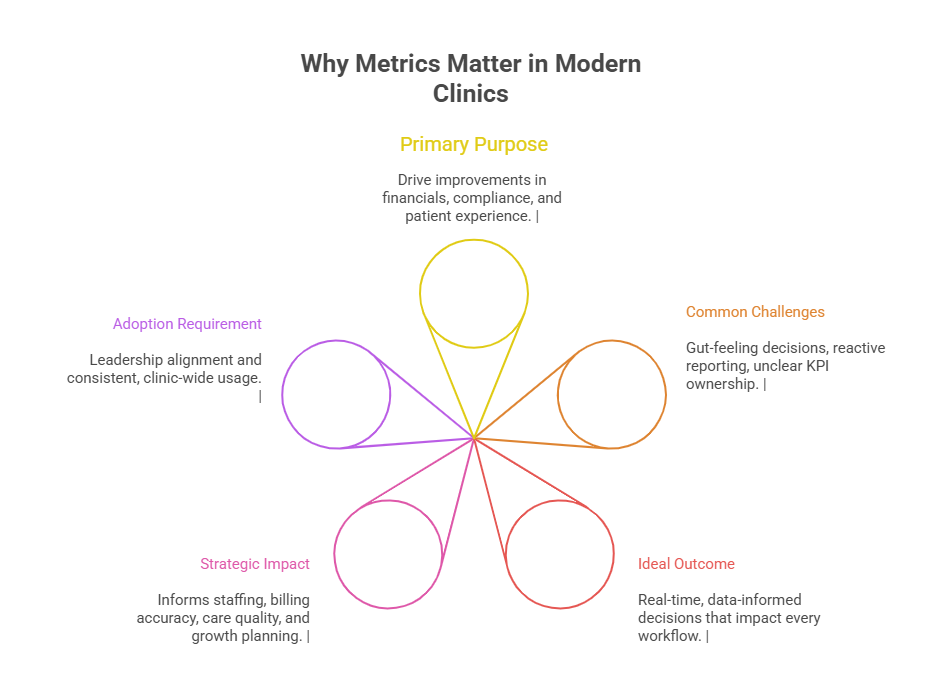
Why Metrics Matter in Modern Clinics
In the healthcare world, what gets measured gets improved. But for most clinics, tracking performance feels reactive—like something you do when revenue drops or patient complaints spike. The reality is, metrics aren't a backup plan. They're the foundation of modern clinical operations. When measured consistently and strategically, metrics become a blueprint for profitability, compliance, and better care. Clinics that invest in tracking KPIs outperform those that rely on gut feeling—by miles.
The most successful practices use performance metrics not just to monitor—but to optimize every layer of workflow: from appointment scheduling and intake to coding accuracy and claim resolution. By identifying operational leaks early, they reduce burnout, increase revenue per encounter, and improve staff retention. Crucially, metrics also provide transparency to payers, patients, and partners—supporting trust, value-based care initiatives, and audit readiness.
Let’s break it down further.
From Efficiency to Profitability
Running a clinic is no longer just about good medicine. It’s about good management. Every wasted minute in a schedule, every missed copay, and every denied claim chips away at margins. Tracking performance gives you control—especially when it comes to financial KPIs like AR days, net collection rate, and charge lag.
AR days (Accounts Receivable days) reflect how long it takes your clinic to collect payments. Industry benchmarks often hover around 30–40 days, but top-performing clinics drive this under 20.
A clean claims rate of over 95% reduces denials and rebilling effort, slashing staff workload while speeding up reimbursements.
Monitoring first-pass resolution rate can reveal payer issues and coding inefficiencies—giving revenue cycle teams the data to act fast.
Financial visibility also empowers clinics to benchmark performance against national standards or specialty-specific peers, helping leadership make smarter growth decisions based on solid data.
Quality, Compliance & Patient Satisfaction
Beyond finances, metrics fuel clinical excellence and regulatory safety. For instance:
Patient wait times, care delivery delays, and follow-up consistency directly impact HCAHPS scores, online reviews, and retention.
Quality-of-care metrics—like missed follow-ups, re-admissions, or treatment plan adherence—offer insight into both care gaps and documentation errors.
Tracking compliance metrics (e.g., HIPAA audit logs, staff training completion, chart closure timelines) helps clinics avoid costly violations and liability exposure.
More importantly, these metrics help build patient-centered care models. When clinics can prove they meet quality benchmarks and offer faster, more responsive service, they don’t just meet expectations—they differentiate themselves in a competitive, consumer-driven landscape.
Key Performance Indicators (KPIs) to Track
Metrics without context are just numbers. The real value of KPIs lies in their ability to drive decisions, reveal inefficiencies, and forecast risk. Whether you're running a solo office or overseeing multiple locations, your ability to compete, comply, and collect hinges on which KPIs you track—and how often. The best-performing medical offices consistently monitor two broad categories of metrics: Revenue Cycle KPIs and Operational KPIs. Let’s break them down.
RCM Metrics (AR Days, Clean Claims)
Revenue Cycle Management (RCM) KPIs are the financial pulse of your practice. They directly impact your cash flow, payer relationships, and administrative burden. Key RCM metrics every practice should track include:
Days in Accounts Receivable (AR Days): This KPI tracks how quickly your clinic gets paid after providing services. The industry target is under 30 days, but many clinics average closer to 45. The longer it takes, the more cash flow stress you face.
Clean Claims Rate: A high clean claims rate (ideally over 95%) means fewer rejections, less staff time fixing denials, and faster reimbursements. Practices with low clean claim rates often see up to 30% of claims delayed or denied due to simple errors.
Denial Rate: This indicates what percentage of claims get rejected. Anything over 5–10% should raise red flags about coding, documentation, or payer rule compliance.
Net Collection Rate: This shows what percent of total collectible revenue is actually collected. Anything under 90% often signals leakage—due to poor follow-up, incorrect coding, or bad debt write-offs.
Monitoring these metrics weekly (not monthly) empowers staff to proactively spot trends, automate rebills, and escalate payor issues before they snowball into long-term revenue loss.
Operational Metrics (Wait Time, Scheduling)
RCM metrics may drive income, but operational metrics drive experience, satisfaction, and scalability. When wait times creep up or appointment slots sit unfilled, the downstream effects hit staff morale, patient retention, and clinical throughput.
Average Patient Wait Time: Longer waits correlate directly with lower satisfaction and higher no-show rates. Aim for under 15 minutes to stay competitive with urgent care centers and concierge clinics.
Scheduling Utilization Rate: This tracks how efficiently your clinic fills its available appointment slots. Rates under 80% may indicate a lack of follow-ups, patient attrition, or front-desk training gaps.
No-Show and Cancellation Rates: Every no-show is lost revenue and wasted clinical time. Effective practices monitor these daily and use automated reminders or prepaid deposits to reduce friction.
Visit Length and Throughput Time: High visit variability may suggest documentation inefficiencies, poor triage protocols, or disorganized rooming workflows.
When operational KPIs are visible and benchmarked, clinics can shift from reactive to proactive mode. They don’t wait for burnout or bad reviews—they use metrics to optimize flow, reduce chaos, and protect patient loyalty.
| KPI Category | Key Metrics Tracked |
|---|---|
| Revenue Cycle Metrics (RCM) | AR days, clean claims rate, denial rate, net collection rate |
| Operational Metrics | Wait time, no-show rate, scheduling utilization, visit duration |
| Clinical & Compliance KPIs | Chart closure timelines, re-admission rates, documentation compliance |
| Measurement Frequency | Weekly or real-time preferred over monthly |
| Benchmarking Use | Compare to internal goals and specialty-based national standards |
Interactive Directory of Tools
Choosing the right tools for performance tracking can mean the difference between data overload and operational clarity. But not every clinic needs an enterprise-grade business intelligence suite. What matters is fit, functionality, and integration. Below is a curated directory of tool types—each tailored to different clinic sizes, needs, and tech maturity.
EHR Dashboards, BI Platforms, Custom Excel Models
From native EHR dashboards to advanced analytics platforms and customized Excel frameworks, every tool listed below empowers clinics to track, analyze, and act on performance metrics without drowning in complexity.
| Tool Name | Category | Best For | Performance Metric Focus | Integration Level |
|---|---|---|---|---|
| Athenahealth Insights | EHR-Embedded Dashboard | Mid-size clinics | AR days, clean claims, patient throughput | Native (within Athena) |
| Tableau Healthcare | Business Intelligence (BI) | Large multi-site facilities | Net collection rate, wait times, compliance alerts | Requires API/ETL sync |
| Power BI + Kareo API | Custom BI Model | Growing practices scaling up | Denial trends, claim resolution, staff efficiency | Moderate integration complexity |
| Google Sheets + Zapier | Low-Code Custom Model | Small practices | Scheduling gaps, no-show rates, chart closures | Manual or Zapier automation |
| Qlik Sense for Clinics | Advanced BI | Data-heavy systems | All KPIs with predictive alerts | Full API & backend integration |
Real-World Use Cases of Performance Tooling
Performance tools only create impact when they’re embedded into real workflows. A dashboard or report means nothing if it’s ignored or misunderstood. Clinics that succeed with tooling are the ones that align usage with clinic scale, specialty needs, and staff habits. This section explores two practical realities: how tooling works in solo vs. multi-site setups—and where most clinics fail during implementation.
Solo Practices vs Multi-Site Facilities
Solo practices need simplicity. Time-strapped clinicians often serve as their own administrators, so tools must offer quick wins with minimal learning curves. For example:
A small family medicine office using Athenahealth’s embedded KPIs can spot claim lags and unpaid balances during lunch breaks. Real-time AR days and rejection dashboards help prevent 90+ day aging spikes—without extra tools or consultants.
A solo chiropractor might rely on Google Sheets with Zapier to auto-log appointment gaps or follow-up delays. With just 30 minutes a month, they can spot whether cancellations are concentrated on a specific day or staff member.
Meanwhile, multi-site groups demand scale and standardization. BI platforms like Tableau or Qlik allow these networks to:
Benchmark provider productivity across locations
Monitor compliance indicators like chart closure rates
Track net revenue per patient by specialty
For these systems, centralized data lakes and API integrations ensure that clinic managers and C-suite execs alike have access to unified, actionable insights—without relying on inconsistent manual reporting from each site.
Common Implementation Mistakes
Even the best tools fail if you skip the groundwork. Clinics most often stumble in four areas:
Tool-First, Strategy-Second: Many buy flashy dashboards before defining their core KPIs. Without a clear performance strategy, tools generate noise instead of clarity.
No Role-Based Ownership: Metrics become “nobody’s job.” AR days might get monitored, but no one is accountable for acting on trends. Effective teams assign KPIs to specific staff roles.
Overcomplicated Interfaces: Front desk teams and providers resist tools that feel like “extra work.” Simplicity and role-specific views drive adoption.
Lack of Change Management: If leaders don’t communicate why the metrics matter, staff see dashboards as surveillance—causing disengagement and even active resistance.
To avoid failure, clinics must treat tool deployment like a clinical rollout—complete with piloting, feedback loops, and team champions. Tools succeed not because they’re powerful, but because they’re adopted, understood, and acted upon daily.
Integration and Training Essentials
Even the most sophisticated performance tool becomes dead weight without seamless integration and proper training. The success of any metrics platform hinges not just on the data it displays—but on how well it fits into your clinic’s daily rhythm. That means aligning software with staff workflows, syncing data sources cleanly, and making sure every user knows exactly how to act on the numbers they see.
Staff Buy-In, API Syncing, Onboarding
You can’t force adoption—you must earn it. The fastest way to fail a performance initiative is to dump a dashboard on your team without context, role-based access, or proper onboarding. Here’s what clinics must do:
Begin with staff education. Before any rollout, clarify why certain KPIs are tracked and how each role (front desk, coders, providers) impacts those numbers. A front desk team tracking no-shows should understand how their actions affect monthly revenue goals and scheduling efficiency.
Leverage API syncing for real-time insights. Whether you're integrating your EHR with a BI platform like Tableau or syncing spreadsheets with billing software via Zapier, real-time sync reduces lag and boosts data accuracy.
Customize onboarding for each user level. Coders need different dashboards than practice managers. Train each team on the few KPIs that matter to their role—no more, no less. That way, the tool becomes useful, not overwhelming.
Use pilot rollouts. Deploy the tool in one department or with one provider first. Gather feedback. Iterate. Only then scale it across the organization. This approach improves adoption while uncovering training or system friction early.
In successful clinics, performance metrics don’t just sit on a screen. They become embedded in morning huddles, monthly reviews, and quarterly planning.
Vendor Support & Update Cycles
The tool is only half the product—the support structure behind it is the rest. If your vendor offers poor response times, confusing documentation, or unclear update schedules, the tool will eventually become a liability. Choose platforms with:
Responsive support teams: Ticket resolution within 24–48 hours ensures your workflow doesn’t stall when bugs or sync issues arise.
Regular update cycles: BI platforms and EHR dashboards must evolve with payer policies, compliance frameworks, and clinical workflows. Ask about update timelines, version controls, and backward compatibility.
Transparent change logs: Clinics need to know what’s changed and how it affects current reports. A surprise UI change can paralyze staff usage overnight.
Accessible training resources: On-demand help centers, video walkthroughs, and dedicated account reps significantly boost staff confidence and tool longevity.
Smart clinics vet vendors not just for tech but for true partnership readiness. Performance tooling isn’t a one-time installation—it’s an evolving process. Your vendor must be prepared to grow with you as your clinic scales, specialties diversify, or compliance requirements shift.
Mastering Clinical Metrics Through Our Medical Scribe Certification
Understanding performance metrics isn’t just for administrators. In today’s data-driven healthcare world, medical scribes play a direct role in quality tracking, documentation compliance, and operational flow. That’s why the Medical Scribe Certification by ACMSO isn’t just about typing notes—it’s about becoming a high-value clinical asset who understands the why behind every metric.
This certification program trains you to:
Identify and document KPIs that directly impact billing, compliance, and physician efficiency—like visit duration, note closure timelines, and encounter coding quality.
Work within EHR systems to ensure that metrics are cleanly captured, minimizing charting errors that can lead to denials or audits.
Support providers by recognizing data that feeds into performance dashboards—including cancellations, patient throughput, and follow-up completion.
By mastering both front-end and backend processes, certified scribes become trusted contributors to clinical performance management. You won’t just capture the visit—you’ll help improve the system behind it.
If you're ready to become indispensable in today’s outcome-driven medical practices, explore the Medical Scribe Certification by ACMSO and take the next step in aligning your skills with the tools that power modern medicine.
Frequently Asked Questions
-
Medical offices should prioritize a blend of financial, operational, and clinical KPIs. At the core are AR days, clean claims rate, denial rate, and net collection rate, all of which affect revenue flow. Operationally, practices must track wait times, appointment utilization, and no-show rates to improve patient throughput. On the clinical side, metrics like chart closure rates, treatment adherence, and quality scores impact regulatory compliance and patient satisfaction. The right combination of these indicators creates a balanced performance profile—enabling smarter decisions across revenue, care quality, and staffing. Clinics that focus on fewer but more actionable metrics typically see the fastest ROI from tooling investments.
-
Small clinics don’t need high-cost dashboards to track performance. Many succeed with customized Google Sheets, free Zapier workflows, and low-code dashboards connected to their EHR exports. These tools allow tracking of no-show rates, daily charges, appointment gaps, and staff productivity with minimal setup. The key is identifying 3–5 core metrics that align with the clinic’s revenue or patient flow challenges. By automating monthly data pulls or even weekly summaries, small teams get real insight without expensive software. With consistency, even a simple spreadsheet model can provide more clarity than underutilized enterprise tools.
-
The most common mistake is using dashboards without clear ownership or action plans. Many clinics track KPIs but fail to assign responsibility. For instance, seeing AR days rise without giving billing staff authority or tools to reduce them results in passive tracking. Another mistake is buying software before defining your KPIs, leading to overcomplicated setups that nobody uses. Lastly, metrics often lack context—teams aren’t trained on how performance affects patient care or revenue, which leads to disengagement. Clinics that succeed treat dashboards like clinical tools—used daily, tied to goals, and owned by someone with decision-making power.
-
Medical scribes play a pivotal role in data accuracy, workflow efficiency, and EHR optimization. With the right training, they don’t just capture what happened—they ensure it’s documented in a way that feeds into performance metrics. For example, accurate timestamps help track visit duration, while standardized note structure improves coding quality and first-pass claim success. Scribes also reduce provider charting time, leading to faster note closure rates and fewer billing delays. The Medical Scribe Certification by Acmso prepares scribes to understand and support core KPIs, transforming them from passive recorders to performance enablers.
-
Warning signs in the revenue cycle include AR days over 40, clean claims rate under 90%, denial rates above 10%, and net collection rates below 90%. Each metric signals friction: long AR days mean delayed payments; low clean claims suggest poor coding or documentation; high denial rates may point to training gaps or payer issues; and low net collection implies billing leakage. Tracking these KPIs weekly (not just monthly) helps catch small problems before they escalate. The best practices use tools that visualize trends over time, not just static snapshots, for proactive RCM management.
-
No—tool compatibility varies drastically depending on your EHR, the tool’s data integration method, and your IT infrastructure. Some EHRs like Athena, eClinicalWorks, or NextGen offer native dashboards. Others may require API-based integration with platforms like Tableau, Power BI, or Qlik. Low-code tools (e.g., Sheets + Zapier) work well for pulling reports via CSV or webhooks. Before choosing a tool, verify its ability to sync with your EHR’s data architecture—ideally in real time. Lack of integration often results in manual exports, data delays, and errors that undermine your ability to take timely action on KPIs.
-
Training must be role-based, use-case driven, and outcomes-focused. Don’t teach everyone every feature—train front-desk staff on scheduling KPIs, billers on claim metrics, and clinicians on documentation quality. Use real examples from your own clinic, not generic templates, and keep sessions short and repeatable. Offer dashboards or views that display only the metrics relevant to each role, and create cheat sheets or short videos for reinforcement. Monthly review meetings help reinforce accountability. The clinics that get results from tooling make performance training a routine—not a one-time event—embedding it into onboarding, reviews, and team meetings.
-
Vendor support is a long-term success factor, not just a purchase point. Good vendors help configure the tool to match your KPIs, train your team, and assist with integration bugs. They also provide update logs, documentation, and API support so your dashboards stay aligned with system changes. Enterprise-grade platforms like Tableau or Qlik offer dedicated customer success managers—but even smaller tools should offer responsive ticketing and live support. The right vendor doesn’t just sell you software—they become a performance partner, ensuring your clinic evolves with new regulatory, payer, and operational realities.
Conclusion
Performance metrics are not a back-office luxury—they’re the backbone of modern clinical operations. Clinics that track and act on the right KPIs see faster reimbursements, stronger compliance, and better patient experiences. But tooling alone isn’t enough. Success depends on choosing systems that align with your workflow, training staff around actionable data, and embedding metrics into day-to-day operations.
Whether you're a solo provider using spreadsheets or a multi-site network running advanced BI platforms, your competitive edge lies in turning numbers into strategy. If you're ready to become a critical force in that transformation, the Medical Scribe Certification by Acmso equips you with the skills to do just that—from documentation accuracy to metric-driven care support.
Use this guide to audit your current tools, align your KPIs with goals, and adopt a performance-first mindset. Your practice—and your patients—will feel the difference.