The Art of Empathy: A CMAA’s Guide to Improving Patient Interactions
Empathy isn’t just a soft skill — it’s the bedrock of meaningful patient care. For Certified Medical Administrative Assistants (CMAAs), showing empathy during appointments, follow-ups, or even phone calls can transform a patient’s healthcare experience. When patients feel heard and respected, compliance improves, anxiety drops, and satisfaction rises. In a time when healthcare can feel impersonal, CMAAs play a critical role in humanizing every interaction.
But empathy in healthcare isn’t a given — it’s a learned, practiced, and refined skill. From navigating cultural sensitivities to recognizing nonverbal cues, mastering empathetic communication is both an emotional intelligence challenge and a practical one. This guide explores what empathy looks like inside real clinics, the barriers CMAAs face, and the exact strategies that elevate patient trust. Whether you’re new to the field or refining your bedside manner, this is your playbook for patient-centered care.
What Empathy Means in a Clinical Setting
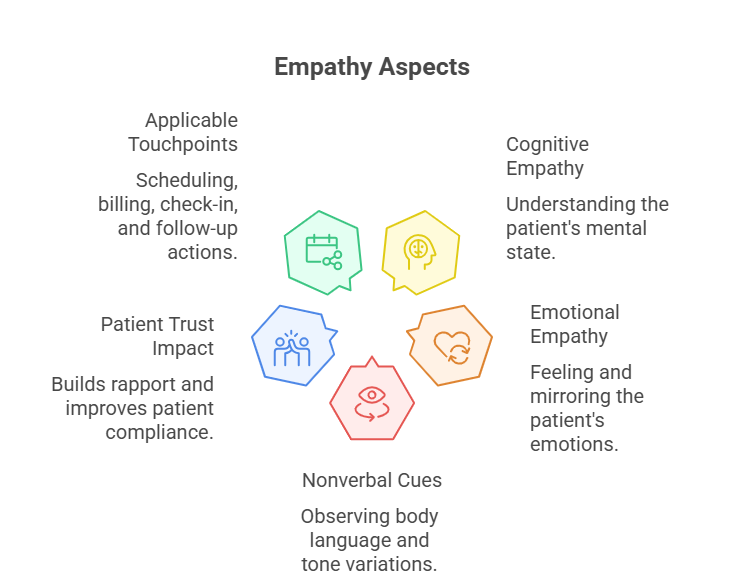
Empathy in a medical environment goes far beyond being “nice” to patients. It’s the ability to accurately perceive and respond to someone’s emotional state — without losing professional boundaries. For CMAAs, this means understanding not just what a patient says, but how they say it, and responding in a way that shows comprehension, respect, and support. It requires listening for tone, watching body language, and using tone-mirroring to de-escalate tension or fear.
Healthcare professionals who demonstrate clinical empathy see measurable results: patients are 1.6x more likely to follow instructions and show increased appointment retention. And it’s not just about bedside care — even during intake, scheduling, or billing conversations, an empathetic tone can defuse frustration and improve cooperation. When empathy becomes embedded in a clinic’s communication style, it directly improves outcomes, patient reviews, and internal morale.
Cognitive vs. Emotional Empathy
There are two primary types of empathy in clinical settings. Cognitive empathy is the ability to understand what a patient is going through — intellectually grasping their condition, emotions, or needs. For instance, knowing that a patient with chronic illness might feel overwhelmed by insurance paperwork is a cognitive recognition.
Emotional empathy, however, is feeling with the patient. It’s the difference between saying “I understand this must be stressful” versus truly conveying that you sense their frustration, fear, or confusion. CMAAs aren’t therapists — but showing emotional empathy in small ways (tone, pace, phrasing) can create a measurable trust bridge between the patient and the care team.
Most CMAAs default to cognitive empathy — especially in busy clinics. But those who develop emotional empathy alongside it create more meaningful, efficient conversations and are seen as more trustworthy by patients and families.
Respecting Patient Fears
Many patients walk into clinics carrying invisible baggage: past medical trauma, financial anxiety, language gaps, or fear of receiving bad news. For CMAAs, acknowledging these fears doesn’t mean prying into personal issues — it means creating space for emotional safety.
This could be as simple as saying, “Take your time — we’ll go step by step,” or avoiding clinical jargon that may intimidate or confuse. It also includes observing non-verbal signs like hesitations, defensive postures, or abrupt tone shifts — and responding with calm clarity and reassurance.
Even minor tweaks — like slowing down speech, asking permission before explaining sensitive procedures, or validating a question — show the patient they are respected, not rushed. Respecting fear is respecting the full human behind the file.
Common Barriers Medical Assistants Face
Even the most empathetic CMAA can struggle to express empathy when workflow pressure, emotional fatigue, or miscommunication gets in the way. Empathy is a skill — but it’s also a resource that can run dry when you’re overwhelmed, understaffed, or misaligned with patient expectations. To improve patient interactions, we must first unpack the most common blocks CMAAs face in real clinical settings.
Time Constraints
In fast-paced clinics, CMAAs often juggle front-desk duties, phone calls, insurance checks, and scheduling — sometimes serving 30+ patients per shift. The result? Conversations get compressed, and empathy becomes a luxury. But rushing can cost more time in the long run. Misunderstood instructions, patient confusion, or frustration can lead to no-shows, errors, or unnecessary rework.
Empathy doesn’t have to take minutes — just moments. Phrases like “Let me make sure I understand” or “We’re here to help you through this” take seconds and diffuse patient anxiety instantly. CMAAs who master micro-empathy — brief, sincere check-ins — make patients feel heard without derailing their schedule.
Cultural Sensitivity
Not all patients express or receive empathy in the same way. A tone that seems warm to one patient may feel invasive to another. Cultural norms affect everything — eye contact, personal space, verbal expression of pain or fear. Without training, CMAAs risk unintentionally offending or confusing patients from diverse backgrounds.
The fix isn’t memorizing every culture — it’s staying alert and curious. Use neutral, inclusive language, avoid slang, and ask clarifying questions rather than making assumptions. If a patient seems uncomfortable, give them time instead of pushing ahead. Cultural sensitivity is about respecting difference, not decoding it.
Clinics that offer diversity and bias training see significant improvements in satisfaction among minority and immigrant patients. CMAAs are often the first point of contact — and their awareness can make or break trust.
Burnout
Empathy fatigue is real. When CMAAs are overworked, emotionally drained, or underappreciated, their emotional bandwidth shrinks. What once felt like compassion can begin to feel like obligation. This leads to short tempers, robotic responses, and rising stress — both for staff and patients.
Combatting burnout starts with recognition. Managers must encourage boundaries, offer wellness breaks, and create safe spaces for feedback and decompression. CMAAs themselves can also use grounding techniques — like deep breathing between patients — to reset.
Empathy doesn’t require emotional overinvestment. It requires presence and intention, both of which are impossible if staff are chronically burned out. Long-term empathy training must include burnout prevention — or it won’t stick.
| Barrier | Challenge Description |
|---|---|
| Time Constraints | Fast-paced environments force CMAAs to rush through interactions, limiting their ability to actively listen and show empathy. |
| Cultural Sensitivity | Lack of training around cultural norms can lead to misinterpretations, discomfort, or unintentional offense during patient interactions. |
| Burnout | Emotional fatigue caused by long hours or emotional overload can reduce a CMAA’s ability to remain empathetic throughout the day. |
| Workflow Pressure | Juggling phones, walk-ins, and paperwork simultaneously causes fragmented attention and robotic communication patterns. |
| Training Gaps | Many clinics lack formal empathy training programs, leaving staff without practical strategies to improve patient connection. |
Proven Techniques to Show Empathy
Empathy isn’t just a feeling — it’s a practice. For CMAAs, the key is turning awareness into consistent action, even during high-stress moments. The following techniques have been proven to boost patient satisfaction, reduce miscommunication, and reinforce clinic professionalism. These aren’t abstract ideas — they’re immediately usable, patient-tested tools that elevate every interaction.
Active Listening
Most patients can tell within seconds whether you’re truly listening — or just waiting for your turn to talk. Active listening means giving full attention to the speaker, reflecting their words, and confirming your understanding. For CMAAs, it starts with eye contact, minimal distractions, and open posture.
Use prompts like “So what I’m hearing is…” or “Let me make sure I’ve got that right…” These brief check-ins prove to the patient that they’re not just a number — they’re a person whose voice matters. Clinics that train staff in active listening report up to 40% fewer misunderstandings during intake and scheduling.
Avoid cutting patients off, even if you think you know what they’re about to say. Letting someone finish builds trust. It signals you respect their time — and their experience.
Validating Patient Concerns
Many patients feel embarrassed, confused, or frustrated when dealing with healthcare systems. When their emotions are dismissed — even unintentionally — it erodes trust fast. Validation doesn’t mean agreeing with everything the patient says. It means acknowledging their feelings without judgment.
Say things like “It’s completely understandable you’d feel that way” or “I hear that this has been really difficult.” Even when correcting a misunderstanding, start by honoring their concern: “I see where the confusion came from. Let me clarify it for you.”
Validation defuses defensive reactions and sets the stage for cooperation. When patients feel seen, they stop pushing — and start listening. This applies to everything from billing disputes to appointment wait times.
Reflective Language Use
One of the fastest empathy boosters is mirroring the patient’s own language — gently and respectfully. If they say, “I’m overwhelmed,” you don’t respond with “You’re fine.” You reflect with “That does sound overwhelming — let’s take it one step at a time.” This technique makes patients feel not just heard, but understood.
Avoid technical jargon when unnecessary. Replace “You’ll need a prior authorization” with “Let me help you get the approval your insurance needs.” This small shift in phrasing reduces confusion and frames you as a patient ally, not a gatekeeper.
Also, match the patient’s pace and tone. If they’re anxious, speak calmly. If they’re quiet, don’t over-talk. Reflective communication aligns your presence with theirs — and shows that you’re tuned in.
Role-Play Scenarios and Training
Empathy can’t be mastered by reading about it — it has to be practiced. One of the most effective ways to train CMAAs in empathetic communication is through structured role-play. These simulations create safe environments where staff can test, refine, and receive feedback on their interactions — before they’re in front of a frustrated or vulnerable patient.
Clinics that implement empathy-focused role-play sessions report up to a 35% increase in patient satisfaction scores. Why? Because real dialogue under pressure reveals blind spots that scripts can’t.
Real-world Dialogue Practice
Generic scripts don’t reflect the complexity of patient communication. Instead, effective role-play uses actual high-stress scenarios CMAAs face daily — like managing late arrivals, de-escalating billing complaints, or navigating difficult disclosures.
Practicing phrases like, “I know this is frustrating — let’s find a solution together,” or “It’s okay to feel overwhelmed. We’ll take this step-by-step,” builds muscle memory for real conversations. CMAAs learn to adjust tone, pacing, and word choice — even when the patient is upset, confused, or non-verbal.
Scenarios can be rotated monthly, focusing on different pain points: elder care, pediatric interactions, new patient onboarding, etc. These short rehearsals sharpen empathy without requiring long training hours.
Involving Supervisors in Review
Role-play without review is just rehearsal. To embed empathy as a standard, supervisors should regularly observe or review scenarios — not to grade performance, but to offer real-time insights. When team leads model empathetic communication and provide constructive micro-adjustments, staff learn faster.
Supervisors might ask: Was the CMAA’s language clear? Did they respond to emotion or just facts? Did they escalate or calm the situation? These reviews allow for continuous improvement, not just one-time training.
Even better: integrate this feedback into staff meetings. Share anonymized wins and lessons. Highlight one technique per week. When empathy is built into the clinic’s learning culture, it stops being a soft skill — and becomes a core competency.
| Training Element | Implementation Strategy |
|---|---|
| Real-world Scenarios | Simulate difficult patient interactions like billing complaints, language barriers, and emotional distress to improve practical empathy responses. |
| Phrasing Practice | Use pre-vetted empathy scripts in rehearsals to build confidence and fluency in calm, validating language during high-pressure moments. |
| Supervisor Review | Supervisors observe or provide structured feedback to help CMAAs improve tone, pacing, phrasing, and emotional presence in mock scenarios. |
| Skill Rotation | Each session focuses on a specific sub-skill like tone matching, reflective listening, or handling anxious patients for skill depth. |
| Team Sharing | Staff debrief together after training to share what worked, challenges faced, and ways to apply new insights in daily workflow. |
Case Studies: Before and After Empathy Training
Sometimes the most powerful proof of empathy’s value comes not from theory, but from real clinic transformations. These case studies show how CMAAs — when trained in practical empathy — can radically shift patient experiences. You’ll see clear differences in tone, outcomes, and patient responses before and after empathy training was implemented.
Elderly Care
Before training: At a suburban clinic, elderly patients regularly expressed confusion during check-ins. Staff used fast-paced language, minimal eye contact, and medical shorthand. One patient left a negative review: “They rushed me, didn’t explain anything. I felt like a number.”
After training: CMAAs were trained to slow their speech, use eye-level posture when speaking, and confirm understanding through teach-back. They adopted phrases like, “Let me walk you through this step-by-step,” and “Would you like me to repeat that?” In 60 days, the clinic saw a 42% drop in complaints from elderly patients — and repeat visit rates improved.
Empathy created clarity, which built trust — and trust drove retention.
Chronic Illness Patients
Before training: Patients managing chronic illnesses (like diabetes or autoimmune disorders) often felt dismissed during administrative conversations. One patient shared, “They didn’t get how exhausted I am. I asked a question about my referral and they just pointed to a number.”
After training: CMAAs underwent scenario-based training tailored to chronic care patients. They learned to recognize signs of fatigue or frustration and used phrasing like, “I know this has been a lot — let’s break it down together.” They also paused to check in emotionally before launching into logistics.
As a result, patient-reported satisfaction jumped by 38% in just three months. These patients no longer felt like they were fighting the system — they felt supported by it.
Empathy didn't just improve conversation flow — it redefined the patient relationship. CMAAs shifted from administrative processors to emotional allies.
How CMAA Certification Boosts Patient Trust
Patients don’t just judge clinics based on the doctors. Often, their first and most frequent contact is with a medical assistant — and whether or not that interaction feels respectful, competent, and empathetic shapes their entire view of care. Certification plays a powerful role in that perception.
When a CMAA is certified through a respected body, patients immediately recognize professionalism. From how calls are handled to how intake forms are explained, certified assistants bring more structure, clarity, and calm. But more than just paperwork — certification reinforces the importance of empathy as a clinical skill, not a personality trait.
The ACMSO CMAA Certification specifically trains medical assistants to balance administrative tasks with patient engagement. The curriculum includes communication strategies, emotional intelligence, and compliance with HIPAA and scheduling protocols. This ensures that every patient touchpoint is handled with both precision and compassion.
In real-world clinics, CMAAs who’ve earned formal certification are consistently rated higher in patient satisfaction surveys. In fact, clinics with fully certified front-desk teams report a 25–30% boost in positive patient reviews — especially around feeling heard, respected, and informed.
A certificate on the wall builds confidence. But it’s what happens behind the desk — the phrasing, the listening, the small empathic touches — that makes certification feel tangible to patients.
People Also Ask
-
Empathy helps CMAAs build trust, reduce patient anxiety, and improve communication outcomes. While the role includes tasks like scheduling and insurance processing, patients often remember how they were treated emotionally, not just logistically. Empathetic CMAAs reduce confusion, prevent conflict, and improve cooperation. This leads to fewer appointment no-shows, clearer patient understanding, and stronger clinic reviews. Even a few words of understanding can calm an overwhelmed patient. Empathy doesn’t slow work down — it makes it more effective. Through role-play and emotional awareness training, CMAAs can learn how to apply empathy in fast-paced clinical environments without sacrificing accuracy or speed.
-
CMAAs develop empathy through structured communication training, scenario simulations, and emotional intelligence modules. Leading programs — like the CMAA Certification from ACMSO — embed empathy into every layer of clinical interaction: intake, phone etiquette, conflict resolution, and compliance. CMAAs are taught to recognize nonverbal cues, use reflective phrasing, and validate patient emotions even in administrative contexts. Clinics often add monthly empathy refreshers and real-world dialogue drills to keep these skills sharp. The goal is to move empathy from theory into daily practice. When staff rehearse complex patient scenarios, it becomes easier to remain calm and clear when tensions rise.
-
Many clinics focus training on compliance, scheduling, and insurance — assuming empathy is either innate or unnecessary at the front desk. But front-desk staff are the emotional gateway to care. If patients feel dismissed, confused, or rushed at intake, that stress carries into the exam room. In high-volume settings, empathy can feel like a luxury. However, research shows that CMAAs who use empathetic phrasing resolve issues faster and reduce complaints. Certification programs like ACMSO’s CMAA course are now emphasizing empathy as a core operational skill, not just a soft skill. Clinics that invest in this training see measurable ROI in patient satisfaction.
-
Yes — dramatically. Multiple studies show that empathetic communication cuts patient complaints by up to 40%. When patients feel heard, they’re more forgiving of long wait times or policy frustrations. CMAAs trained in empathy use reflective phrases like, “I can see why this feels frustrating,” followed by a solution-oriented approach. These micro-moments de-escalate tension. Clinics that roll out empathy training often track a noticeable drop in front-desk conflicts, call escalations, and online negative reviews. And because most complaints stem from poor communication — not medical error — CMAAs have a direct opportunity to shift outcomes through empathy.
-
Effective empathy phrases are short, sincere, and focused on validation. Examples include:
“I understand this may feel overwhelming. Let’s take it one step at a time.”
“That sounds frustrating — let me see how I can help.”
“You’re not alone in feeling that way. We handle this often, and I’ll walk you through it.”
These phrases do more than soothe — they reframe the conversation around patient support. CMAAs should also practice mirroring tone and pacing, especially with anxious or elderly patients. Certification programs like the one from ACMSO train CMAAs in using these phrases fluently and naturally.
-
Empathy acts as a de-escalation tool. When patients are upset, logical explanations rarely work unless their emotions are first acknowledged. CMAAs who respond with “I hear that you’re frustrated” rather than “That’s just our policy” immediately reduce resistance and invite cooperation. This opens space for a more productive exchange. Empathy doesn’t mean agreeing — it means recognizing emotion before addressing facts. Certified CMAAs, especially those trained through ACMSO, learn to manage emotional tone while staying within clinic protocols, helping prevent conflicts from spiraling. Empathy turns emotionally charged moments into opportunities for reassurance and clarity.
-
Empathy training isn’t just about individual performance — it reshapes clinic culture. Long-term benefits include:
Improved patient retention
Stronger online reviews
Higher morale among front-desk staff
Fewer miscommunications with clinical teams
CMAAs who undergo empathy training feel more confident and respected, which reduces turnover. Patients also become more cooperative and trusting, which improves workflow and reduces delays. Clinics that embed empathy into onboarding and ongoing training — like those using the ACMSO CMAA Certification — see better patient outcomes and stronger team cohesion. Empathy isn’t a temporary fix — it’s a strategic advantage.
Our Verdict: The Competitive Edge of Empathy
Empathy isn’t optional — it’s a differentiator that patients feel immediately. For CMAAs, empathetic communication is what turns rushed check-ins into respectful dialogue, and policy explanations into moments of clarity. Clinics that prioritize empathy don’t just improve satisfaction scores — they build lasting patient trust and team resilience.
The best part? Empathy is teachable. Through structured training, real-world simulations, and certification programs like ACMSO’s CMAA, medical assistants can build the confidence to handle any patient scenario with calm, clarity, and compassion. In a healthcare system that often feels cold, empathy is the warm skill that delivers hard results. For CMAAs looking to stand out — and for clinics looking to lead — empathy is the edge that endures.