How to Master Patient Chart Audits in EMR Systems
Patient chart audits are essential to clinical accuracy, risk management, and regulatory compliance — but mastering them inside modern EMR systems requires more than just clinical know-how. For medical scribes, audits represent both a responsibility and an opportunity to prove documentation quality and workflow precision. As the digital backbone of today’s healthcare, EMRs contain clues that reveal errors in coding, gaps in charting, and potential red flags for reimbursement or legal action. If you're not trained to catch those — you’re not audit-ready.
This is where EMR audit mastery becomes critical. A well-trained medical scribe doesn’t just document — they understand how to think like an auditor. From reviewing chart completeness and identifying missing signatures to recognizing EMR log anomalies, every detail matters. That’s why the Medical Scribe Certification by ACMSO includes in-depth training on real-world EMR audit cases — so you don’t just learn what to document, but how to defend it under scrutiny. This guide breaks down every step of the process — so your audits aren’t just good, they’re bulletproof.
What Are Patient Chart Audits & Why They Matter
Patient chart audits are structured reviews of clinical documentation within an EMR to assess accuracy, completeness, and compliance. These audits aren’t random—they're strategic evaluations of how well a provider’s documentation aligns with clinical guidelines, billing codes, and legal standards. For medical scribes, understanding audits is non-negotiable: your entries are often the first layer of data that auditors inspect.
A well-conducted audit can identify whether documentation supports the billed service level, whether signature authentication is valid, or whether time-stamped entries match the clinical activity performed. When discrepancies are flagged, they can lead to denied claims, regulatory penalties, or worse—liability exposure during malpractice reviews. But when done right, audits strengthen a provider’s compliance posture and ensure payer confidence in documentation accuracy.
Audit Types: Retrospective, Prospective, Concurrent
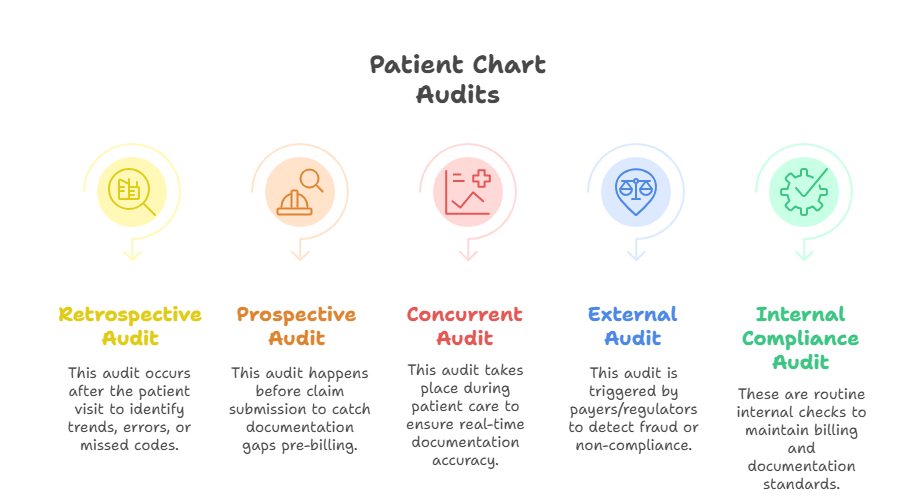
Retrospective audits review patient charts after the care has been delivered. These are the most common type used in quality assurance, coding accuracy checks, or post-payment audits. They help detect patterns like under-documentation or late entries, giving practices a chance to improve.
Prospective audits are conducted before the provider submits documentation or billing. These are proactive, especially in training environments, ensuring that what gets submitted is correct. They reduce downstream errors but require quick turnaround from reviewers.
Concurrent audits happen while the patient is still receiving care, often in inpatient or hospital settings. Auditors or compliance staff might review ongoing documentation in real time, offering on-the-spot corrections to avoid systemic errors or policy breaches.
Each type plays a role. Scribes trained under the Medical Scribe Certification by ACMSO are equipped to understand how to adapt documentation to survive each format — from post-discharge reviews to real-time compliance checkpoints.
Regulatory and Internal Drivers
Audits aren’t optional — they’re mandated or triggered by multiple stakeholders:
Regulatory bodies (e.g., CMS, OCR, HIPAA enforcement teams) often audit randomly or when anomalies are flagged in claims.
Internal compliance teams perform audits to maintain standards across physicians, reduce legal exposure, or train new staff.
Private insurers may initiate targeted audits when billing patterns suggest upcoding or inconsistent clinical documentation.
Medical directors rely on audits to ensure staff follow evidence-based documentation standards.
For scribes, understanding why an audit is happening helps you document more defensibly. The Medical Scribe Certification by ACMSO teaches not just what to enter, but how to structure notes for audit resilience — a skillset that separates you from entry-level scribes and puts you in line for senior roles.
Structuring an Effective Audit Process
Audits aren’t one-size-fits-all. An effective audit process in an EMR system starts with structure — knowing what to review, how often, and why those records were selected in the first place. Medical scribes who understand this framework operate with more confidence and accuracy, becoming trusted members of the compliance workflow.
Audit workflows should be standardized, so every record gets reviewed under consistent criteria. This includes defining which provider types or services are under review, whether it's tied to a billing code range or specific diagnosis category, and how discrepancies will be escalated. Without this structure, audits become unreliable and subject to reviewer bias or inconsistency.
High-functioning audit processes rely on collaboration between compliance officers, coders, providers, and scribes. Everyone must understand their role, and scribes are at the front line. The Medical Scribe Certification by ACMSO equips you with the framework to understand, participate in, and act on EMR audit results confidently.
Sampling Criteria and Record Selection
The first audit decision: which records to pull. Smart audits never review all records — they use sampling methods that balance volume with representativeness:
Random sampling ensures impartiality but may overlook high-risk charts.
Focused sampling selects records based on risk signals like high RVU codes, recent denials, or new providers.
Statistical sampling uses formulas to select a mathematically valid subset, often for payer audits.
The key is defining the sample before the review, not during. For example, a practice may audit 10 patient encounters per provider per month using focused sampling on high-level E/M codes. Scribes should document with this structure in mind, ensuring every chart meets billing, signature, and content completeness standards.
Audit Timelines and Frequency
Audit timing is critical. Delays in post-service reviews reduce the window to make corrections or rebill claims. Here’s what efficient timelines look like:
Prospective audits should be completed within 24–48 hours of documentation.
Retrospective audits should occur monthly or quarterly, with reports issued within 5–10 business days.
Concurrent audits are continuous and often flagged by EMR alerts or compliance dashboards.
Set a recurring audit schedule per department or provider. Frequency might vary based on performance: new staff or high-risk specialties may be audited more often. Ensure there’s a process for urgent escalation if errors affect patient safety or billing fraud flags are raised.
| Element | Best Practice | Why It Matters |
|---|---|---|
| Sampling Method | Focused or statistical sampling | Targets high-risk or representative records |
| Record Selection Criteria | Risk level, code range, provider group | Keeps audits relevant and efficient |
| Audit Frequency | Monthly or quarterly based on risk | Prevents backlog and promotes consistency |
| Audit Documentation Tools | EMR filters, audit views, report generators | Streamlines review and highlights problem areas |
| Post-Audit Action Plan | Standard correction and feedback loop | Ensures learning and reduces repeat issues |
What to Look for During Chart Reviews
Knowing what to look for during a chart review is what separates checkbox audits from high-impact, risk-reducing audits. Medical scribes play a key role in creating documentation that stands up to these reviews. Whether the audit is triggered by a payer, compliance team, or internal QA, every chart should be reviewed for technical completeness, clinical coherence, and billing defensibility.
What makes EMR audits different from paper reviews is their volume and complexity — every click, every timestamp, and every dropdown selection can be part of the audit trail. The scribe’s responsibility isn’t just to transcribe — it’s to ensure the note reflects exactly what happened, in the correct format, with the right metadata. That’s why the Medical Scribe Certification by ACMSO dedicates modules to chart reviews: it’s where your documentation skills get stress-tested.
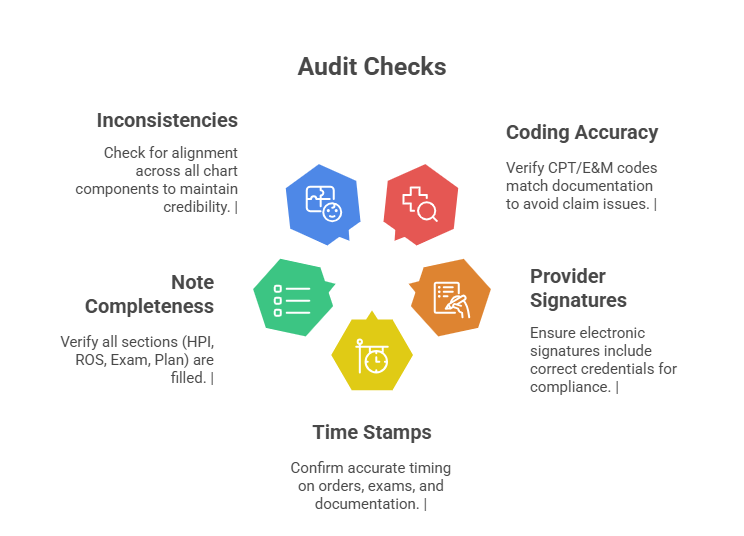
Coding Accuracy, Signatures, Completeness
Three core elements make or break an audit:
Coding accuracy: The documentation must match the billed CPT and ICD-10 codes. If the physician documents a level-4 visit but the scribe omits a required ROS section, downcoding or denials may follow. Always cross-reference coding guidelines for each visit type.
Signatures and time stamps: All entries must be signed, dated, and electronically time-logged by the appropriate user. Missing or delayed authentication can flag a chart as incomplete.
Note completeness: EMRs make it easy to skip required elements. Make sure documentation includes HPI, ROS, exam, assessment, plan, and required attestations. Incomplete charts are audit targets.
Your job isn’t just to enter what’s dictated — it’s to ensure the documentation has enough clinical detail to justify medical necessity and survive scrutiny.
Red Flags and Risk Indicators
Auditors don’t just look for what's present — they also hunt for what’s missing, inconsistent, or suspicious. Here's what raises red flags:
Cloned notes across multiple patients or visits
Mismatch between assessment and plan (e.g., treating hypertension but not documenting it)
Inconsistencies between vitals, chief complaints, and physical exams
Overuse of high-level E/M codes without corresponding complexity
Frequent addendums or late entries
As a medical scribe, learn to recognize and flag patterns that could cause audits to fail. Every section you help write should make the provider’s clinical reasoning crystal clear.
Tools and EMR Features That Make Audits Easier
You can’t master patient chart audits without mastering the EMR features built to track, flag, and surface documentation errors. Most audit bottlenecks stem from users not knowing how to fully leverage the system’s built-in tools — or worse, bypassing them entirely. As a medical scribe, knowing what tools exist (and how to use them) makes your documentation more audit-resistant, efficient, and legally defensible.
Some features are obvious — like signature prompts. Others are underutilized but critical: like audit trails, note version histories, and provider productivity dashboards. These aren’t just IT conveniences. In audit scenarios, they become evidence artifacts that either protect or penalize a provider. That’s why the Medical Scribe Certification by ACMSO ensures scribes get hands-on exposure to these systems — not just theory, but real-world EMR tool practice.
Audit Logs, Reports & EHR Filters
Audit logs are the black box of EMRs. They track who accessed what, when, and whether the chart was edited post-visit. This is crucial during audits triggered by malpractice claims, compliance reviews, or payer disputes.
Use report builders or customizable audit views to identify missing notes, unsigned entries, and conflicting codes.
Many systems have filter options to isolate visits by date, CPT level, modifier usage, or diagnosis group — allowing for quicker sampling during internal reviews.
Time-stamp comparisons between order entries, documentation, and prescriptions reveal workflow gaps or compliance issues.
Scribes must know how to generate and interpret these reports. These tools also help flag discrepancies before they ever become compliance violations.
Third-party Audit Tools That Sync With EMRs
Not all audits happen inside the EMR. Many organizations use third-party compliance tools that integrate with major EMRs like Epic, Cerner, or eClinicalWorks. These platforms extract structured data to perform more complex rule-based audits or predictive error modeling.
Popular tools include:
Compliance tracking platforms (e.g., ComplyMD, MDaudit) that automate scoring and assign risk profiles
NLP-based scrubbing tools that compare dictated text to billing codes for gaps
Pre-bill validators that halt claims if documentation doesn’t meet billing rules
The key is interoperability. These tools often run side-by-side with EMRs and can scan thousands of charts quickly — meaning your documentation will be scrutinized algorithmically before a human ever looks at it.
| Tool or Feature | Functionality | How It Helps in Audits |
|---|---|---|
| Audit Logs | Tracks access, edits, and timestamps | Provides traceability for legal defense |
| Custom Reports | Filters records by CPT, provider, date | Speeds up audit sample selection |
| Note History | Shows all edits and who made them | Verifies timing and authorship |
| Third-Party Sync Tools | Auto-scan charts using audit rules | Flags issues before submission |
| Alerts and Prompts | Reminders for unsigned notes or missing elements | Reduces documentation gaps proactively |
Post-Audit Steps & Continuous Improvement
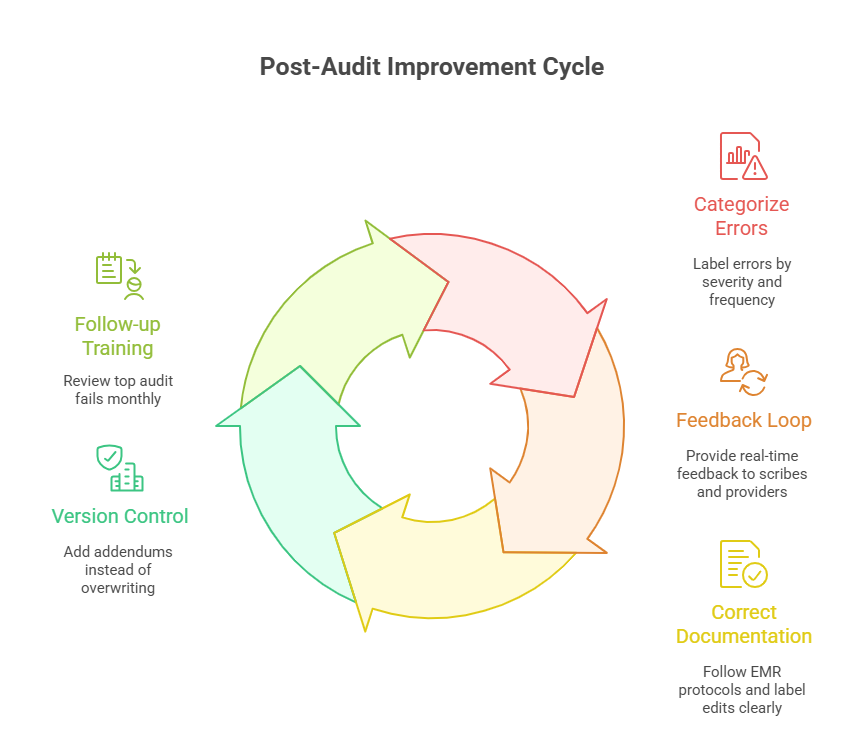
Completing the chart audit is only the midpoint. The real impact of an audit lies in what happens next — how findings are communicated, errors corrected, and workflows refined. Without a structured post-audit strategy, even the most accurate reviews will lead to minimal change. For medical scribes, post-audit phases are opportunities to identify documentation blind spots and evolve their accuracy and speed in real time.
This is where audit reports transform from compliance exercises into training blueprints. Teams that implement consistent feedback cycles and timely documentation corrections significantly reduce repeat errors. That’s why the Medical Scribe Certification by ACMSO trains scribes not only to document well — but to respond constructively to audit findings, using them as a lever for ongoing skill development.
Error Reporting and Staff Feedback Loops
Audit reports must be actionable. They should do more than list what went wrong — they should trigger concrete feedback loops that reach scribes, providers, coders, and medical administrators. Here’s how high-functioning teams manage it:
Error categorization: Flag errors as minor (e.g., missed checkboxes) or major (e.g., unsupported codes, conflicting data). This helps prioritize corrections.
Scribe-specific feedback: If a documentation error stems from how the scribe recorded the visit, that feedback must go directly to them — clearly, promptly, and with a training resource attached.
Real-time flagging: Many EMRs allow reviewers to insert inline comments or create audit dashboards visible to specific users. This shortens the time between mistake and correction.
Feedback sessions: Monthly or bi-weekly reviews help the whole team spot recurring trends, such as missed elements in HPI or signature delays.
Feedback loops aren’t punitive — they’re preventive. They build muscle memory and reduce future audit risk.
Documentation Corrections and Follow-Ups
Correcting documentation after audits involves more than editing a note. It requires:
Version tracking: Always preserve the original chart version, especially in legal-risk environments.
Late entries and addendums: These must be labeled appropriately and time-stamped clearly. Avoid backdating.
Sign-off validation: Providers must electronically sign all corrections to affirm they reviewed and approved the changes.
Billing adjustments: If the correction affects CPT or ICD-10 coding, communicate with the billing team immediately to stop, correct, or resubmit claims.
Scribes involved in the correction process must know when to act — and when to escalate. The Medical Scribe Certification by ACMSO teaches this escalation logic as part of audit-based case simulations.
Certification That Trains You in Real-World Auditing
Most scribes enter the field thinking documentation is just about speed and accuracy — but few realize how often their notes become the foundation of clinical audits. Without audit readiness, even well-documented notes can fall apart under scrutiny. That’s why the Medical Scribe Certification by ACMSO doesn’t stop at basic charting — it trains you to think, write, and review like an auditor from day one.
The program includes audit-heavy modules that simulate real-world compliance reviews. You don’t just learn what fields to complete — you learn why each field matters in retrospective and concurrent audits. You'll work through live case documentation samples that mirror payer audits, internal quality reviews, and even malpractice-prevention audits, all inside structured EMR workflows.
Here’s what sets the training apart:
Live case audits: Review flawed charts, correct them, and explain each fix based on real compliance rules.
Coding alignment drills: Match documentation to CPT/E&M codes and learn to spot mismatch errors before they trigger claim denials.
Signature & timestamp protocols: Get drilled on legal signing requirements, edit tracking, and addendum integrity.
Audit simulation exercises: Work through scenarios where your documentation faces scrutiny from coders, insurers, and compliance officers.
This isn’t passive learning. You’ll actively write, analyze, and defend notes under conditions that match the real job. It prepares you to not only avoid audit flags but also to collaborate with compliance teams, respond to feedback, and continuously refine your charting habits.
Graduates of the Medical Scribe Certification by ACMSO often move into senior scribe, compliance assistant, or EMR analyst roles faster — because they come audit-ready. They don’t just document what’s dictated; they document with the audit lens already in mind. That’s the difference between basic scribing and professional-grade EMR documentation.
Frequently Asked Questions
-
The main goal is to verify that clinical documentation is accurate, complete, and compliant with billing and legal standards. In EMR systems, audits ensure that what was charted reflects actual patient care and supports medical necessity. Auditors look at coding alignment, provider signatures, time stamps, and whether required elements like HPI, ROS, and assessments are present. For medical scribes, audits are the ultimate quality check. If you’re trained through the Medical Scribe Certification by ACMSO, you’ll know how to document in ways that consistently pass both internal and external audits.
-
Chart audits are conducted by compliance officers, coding specialists, internal QA teams, or external third-party auditors. In hospitals, the compliance department might run concurrent audits during patient stays, while private practices may hire auditors to do retrospective reviews. Insurance companies can also trigger audits if billing patterns seem suspicious. As a scribe, you won’t conduct audits directly, but your documentation will be audited — often in real time. The Medical Scribe Certification by ACMSO teaches you to anticipate what auditors look for, so your notes never raise red flags.
-
Modern EMRs come equipped with features like audit logs, report builders, and note history trackers that make audits faster and more precise. You can filter charts by provider, diagnosis, or CPT code to review patterns, generate missing signature alerts, or identify unsigned notes. Many systems also allow version tracking, so you can compare edits over time. These tools aren't optional — they're central to audit accuracy. The Medical Scribe Certification by ACMSO trains students on real EMR systems so they can use these tools efficiently from day one.
-
The most frequent audit errors include missing provider signatures, mismatched codes, cloned notes, and incomplete SOAP elements. Auditors often catch discrepancies between the exam and assessment or signs that a scribe copy-pasted templates without customizing. Notes that don’t justify the billed service level are also red flags. Even something as small as a late entry without a time-stamp label can lead to a failed audit. Training programs like the Medical Scribe Certification by ACMSO teach scribes how to avoid these pitfalls and protect providers during audit review.
-
Scribes can support documentation correction, but only providers can make clinical edits or sign-offs. However, scribes can flag issues, prep corrections, or add clearly labeled late entries with proper time stamps and disclaimers. They must also follow EMR-specific policies for version history and corrections, ensuring all changes remain audit-compliant. Corrections should never involve backdating or overwriting original content. The Medical Scribe Certification by ACMSO includes modules on audit responses, helping scribes understand how to properly assist in post-audit revisions and escalate serious issues.
-
The frequency of chart audits depends on practice size, specialty, and risk exposure. High-risk areas like cardiology or pain management may need monthly audits, while low-risk departments may do them quarterly. New hires or providers with prior audit issues are often audited more frequently. EMRs can schedule automated audit triggers based on time or billing codes. For scribes, this means their work will be under routine scrutiny. The Medical Scribe Certification by ACMSO prepares you to document in a way that passes audits regardless of frequency.
-
To make your documentation audit-proof, ensure every note is specific, complete, and aligned with coding and billing standards. Avoid using generic templates or omitting required sections like ROS or Plan. Double-check for missing provider signatures, inconsistent time stamps, or incomplete encounters. Document exactly what’s dictated, but use your training to structure it in an audit-ready format. The Medical Scribe Certification by ACMSO teaches scribes to think like auditors — so every note is defensible, even under the most detailed review.
-
Yes — scribes with formal audit training are in high demand, especially in larger systems, surgical centers, or revenue cycle teams. They reduce legal risk, improve claim approvals, and streamline provider workflows by ensuring first-time documentation accuracy. Many employers now prefer candidates who’ve completed programs like the Medical Scribe Certification by ACMSO because it demonstrates not just EMR fluency but also a strong grasp of compliance, error prevention, and audit survival. This training can lead to faster promotions into QA, billing, or documentation leadership roles.
Summing Up: Patient Safety Starts Here
Mastering patient chart audits is about more than compliance — it's about protecting patient safety, ensuring accurate clinical communication, and supporting financial integrity in every encounter. In the digital era, where EMRs capture every action, scribes play a direct role in how defensible and audit-ready the record becomes. A single documentation misstep can trigger denials, liability, or care delays — but a well-trained scribe can prevent all of it.
The key is fluency: knowing how to document, spot red flags, use EMR tools, and understand audit frameworks inside and out. That’s what the Medical Scribe Certification by ACMSO delivers — a career-ready foundation that doesn’t just teach how to enter data, but how to audit-proof every word. Whether you're new to scribing or ready to advance, this is where smart documentation begins — and where audit risk ends.
| Poll Question | Your Answer |
| Which EMR audit feature do you find most useful? |