EMR Security Best Practices Every Medical Assistant Should Know
Electronic Medical Records (EMRs) are now the backbone of every modern clinic—but security failures almost always begin at the administrative level. In 2025, cyberattacks don’t always start with complex hacking—they start with a missed logout, a reused password, or a mismanaged access point. As a medical assistant, your daily routines directly influence the safety of every patient record in the system.
Whether you’re handling scheduling, intake, or documentation, your choices define your clinic’s data protection posture. This guide breaks down actionable, real-world EMR security practices every certified assistant must apply. From access control to remote logins and audit flags, you'll learn what truly matters. And if you're new to EMR systems, begin with this Complete Guide to Electronic Medical Records for Assistants to understand how different features and functions affect day-to-day workflows—and why security starts with you.
Why EMR Security Starts With You
The Admin’s Role in EMR Risk Exposure
Security doesn’t fail because of complex code—it fails because of simple habits. Medical assistants control the first line of defense in every EMR system. One forgotten logout, one shared login, or one careless click can expose hundreds of records. Most real-world breaches happen not from hackers breaking in, but from admin-side missteps—such as accidentally leaving a screen open or using default passwords. The moment you log in, your actions either protect or expose sensitive patient data.
HIPAA and CMAA-Aligned Security Expectations
HIPAA outlines clear zones of responsibility that directly involve administrative staff. This includes secure logins, workstation usage, data transmission, and mobile access. Even failing to properly dispose of printed EMR data can be a violation. Medical assistants need to know their role in maintaining compliance and audit-readiness. To fully understand your responsibilities under HIPAA in daily medical settings, refer to HIPAA Simplified: Everything Medical Admin Assistants Need to Know—it’s a foundational resource every CMAA should bookmark.
Every medical assistant action inside an EMR—whether it’s login hygiene, logout timing, or handling printed records—affects patient privacy. Most breaches begin with overlooked habits, not sophisticated hacks.
HIPAA and CMAA frameworks hold admin staff directly accountable for these front-line exposures. If you touch a terminal, transmit data, or access patient records, you’re a core part of the risk surface—and the solution.
Passwords, Permissions, and Patient Privacy
Managing Passwords Without Weakness
In EMR security, weak passwords are equivalent to unlocked doors. Medical assistants must use multi-factor authentication, rotate credentials regularly, and ensure systems automatically lock after periods of inactivity. Password vaults approved by IT can simplify credential management without sacrificing control. Never write down logins, and always logout—especially when switching terminals. The faster your routine becomes, the easier it is to miss these critical steps.
Role-Based EMR Access Rules
EMRs segment user access based on defined job roles. Assistants shouldn’t have access to everything, and “least privilege” is the standard. This means access should be restricted to only what’s essential for the task—no more. Lab results, progress notes, and billing access are often tiered. Understanding these access levels protects both the clinic and the assistant. For more on how EMRs define and manage these permission tiers, see the Complete Guide to Electronic Medical Records (EMR) built specifically for support staff like CMAAs.
| Topic | Details |
|---|---|
| Managing Passwords | Use multi-factor authentication, rotate passwords regularly, and enable auto-lock after inactivity. Never write down credentials or leave a session open. Consider using IT-approved password vaults. |
| Access Control Rules | EMRs enforce role-based permissions. Access should follow the "least privilege" model—assistants should only see what they need (e.g., vitals, notes) but not sensitive diagnostics or billing unless necessary. |
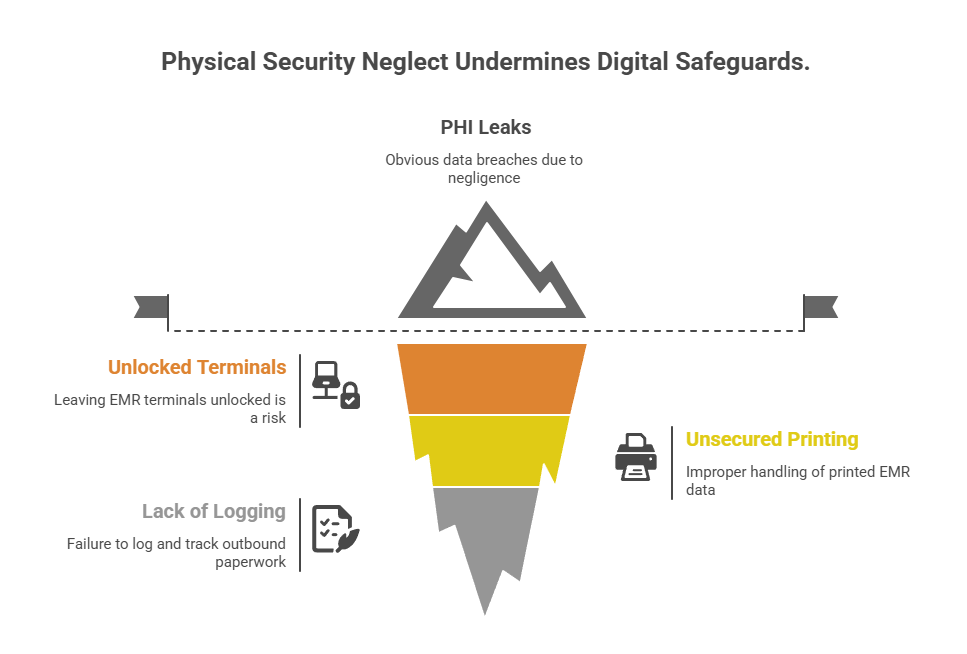
Physical Security in Digital Systems
Guarding Workstations and Shared Terminals
Even with perfect software protocols, physical exposure can undo everything. Medical assistants must never leave EMR terminals unlocked—not during short conversations, not during quick walks to the printer. Every shared screen must auto-lock, require ID badge access, and display user session logs to verify who last accessed it. Clinics often overlook physical security, but it remains one of the most common PHI leak points. Learn how this plays out in actual shared system environments with EMR Software Terms – Interactive Dictionary & Walkthroughs, which breaks down security triggers in real-time workflows.
Printer, Fax, and Physical Chart Handling
Printing EMR data brings digital data into vulnerable physical space. Always verify recipients before sending faxes, never leave printed charts unattended, and shred all PHI copies immediately. Print queues must be cleared after each use to avoid mix-ups or unauthorized pickups. Assistants must also label and log outbound paperwork, especially when it involves referrals, lab results, or prescriptions. Failing to handle paper trail security makes the best EMR systems worthless.
Red Flags Medical Assistants Must Catch in Real-Time
Signs of Unauthorized Access
You don’t need a firewall to spot red flags—you need awareness. If a chart is being accessed at odd hours, or from a department not assigned to that patient, that’s suspicious. Frequent edits to a patient’s record by different assistants could also indicate a breach. Assistants should review session logs and report anomalies immediately. Modern EMR systems now offer built-in audit tools, and How to Master Patient Chart Audits in EMR Systems gives CMAAs step-by-step insights on identifying these risks before IT even notices.
Suspicious Patient or Staff Requests
Sometimes, the breach walks in through the front door. “Can you just print this for me without logging it?” or “Don’t tell the doctor yet, I just want to check” are clear signals something is off. Assistants must be empowered to say no and escalate. This protects both the patient and the clinic from violations, fraud, or legal action. Every CMAA must learn to identify manipulation—because social engineering remains the easiest breach tactic in 2025.
Red Flags Medical Assistants Must Catch in Real-Time
Signs of Unauthorized Access: Unusual chart access patterns—like late-night logins, frequent edits by multiple assistants, or mismatched department views—are red flags. Review session logs and use built-in EMR audit tools to catch these issues early.
Suspicious Patient or Staff Requests: Requests to bypass logging, avoid physician review, or manipulate documentation should be treated as potential security threats. CMAAs must confidently escalate these attempts to uphold privacy and compliance.
Best Practices for Remote and Cloud-Based EMR Use
Secure VPNs and Device Control
Cloud-based EMR systems offer flexibility—but they also widen the threat surface. Medical assistants must only use clinic-issued devices, secured with endpoint protection and encrypted VPN tunnels. Personal devices or open networks (like public Wi-Fi) should never be used for accessing patient data. Cloud platforms often track access logs—use them daily. For reference, explore how cloud-native systems have changed workflows in Cloud-Based EMRs: 10 Systems Revolutionizing Medical Administration. It offers context on securing modern, remote-friendly medical office setups.
Remote Login Hygiene
Never stay logged in beyond a task. Remote access requires extreme discipline: always log out, never save passwords in browsers, and use screen protectors in shared spaces. If assistants step away—even for a moment—they must ensure screens are locked. Clinics must enforce these habits just as strictly as in-office protocols. One careless session can expose hundreds of records, especially in multi-practice systems using centralized EMRs.
How confident are you in your remote EMR login habits?
Tools That Enhance EMR Security Without IT Help
Admin-Led Safeguards
Not every solution requires an IT ticket. Assistants can enforce critical safeguards on their own: activate inactivity timeouts, disable USB data ports, restrict file downloads, and place visible privacy signage in all terminals. Proactivity reduces the chances of on-site leaks. Clinics must standardize these rules—but assistants must uphold them. These habits make a difference every day, especially in open-floor clinics with rotating staff.
Platforms That Empower CMAAs
Some EMR platforms now give non-technical staff access to audit dashboards, showing login history, active users, and real-time flags. These tools empower CMAAs to help monitor for suspicious activity, especially in understaffed practices. When comparing platforms, prioritize those with built-in security dashboards. EMR Software Comparison Guide: Choosing the Right System for Your Medical Office breaks down which systems best support assistant-level security enforcement.
| Key Area | Details |
|---|---|
| Admin-Led Safeguards | Assistants can enable inactivity timeouts, restrict file downloads, and disable USB ports without IT help. These steps reduce on-site security gaps, especially in shared workstations. |
| Visible Privacy Measures | Posting signage near terminals, covering monitors, and using keyboard shields helps prevent shoulder-surfing and accidental exposure of PHI. |
| Audit Dashboard Access | Modern EMRs offer user-level dashboards for assistants to view login logs, session activity, and trigger real-time alerts—no admin rights required. |
| Assistant-Centered Platforms | Choose systems designed with CMAAs in mind—ones that allow assistants to maintain security visibility without relying entirely on IT teams. |
Why ACMSO Medical Scribe Certification Embeds Security Deeply
Security Training in Every Module
The ACMSO Medical Scribe Certification doesn’t treat EMR security as an afterthought—it’s embedded into every module. Assistants learn the importance of access control, PHI documentation boundaries, and real-world breach scenarios through guided walkthroughs. Whether entering SOAP notes or managing referrals, students are shown how to spot and prevent common vulnerabilities. The entire certification structure is built around preparing assistants for actual breach points, not just theory.
HIPAA-Aligned Simulations and Real Scenarios
ACMSO goes beyond textbook learning. It provides interactive simulations that mirror real clinical settings: securing terminals in busy practices, responding to unauthorized requests, and preventing miscommunication that could leak PHI. Modules are aligned with core HIPAA expectations for medical administrative support. These scenarios bring to life what most courses skim over. See how security is applied during EMR use in Step-by-Step Guide to Efficient EMR Data Entry for Medical Admins.
Becoming a Leader in EMR Responsibility
Today’s clinics need more than just scheduling support—they need EMR defenders. The ACMSO credential shows employers that graduates understand PHI regulations, platform nuances, and internal protocol enforcement. Assistants with this training enter clinics ready to lead in audit prep, workstation policy, and data integrity. Certification is no longer a bonus—it’s proof of security readiness from day one.
Final Thoughts
Electronic Medical Record security isn’t just an IT concern—it’s a daily responsibility for every medical assistant. The best encryption protocols and enterprise-grade EMR software can’t compensate for admin-side gaps like weak passwords, shared logins, or ignored audit trails. In 2025, clinics are increasingly prioritizing security awareness and protocol fluency when hiring for administrative roles.
By mastering the habits outlined in this guide and earning your credential through the ACMSO Medical Scribe Certification, you don’t just support EMRs—you defend them. Your training, vigilance, and certification signal to employers that you’re ready to be trusted with digital patient care from day one.
Frequenlty Asked Questions
-
The most common mistake is leaving EMR systems open and unattended. Even with strong passwords and encrypted software, unlocked workstations or shared logins can lead to massive HIPAA violations. Assistants often multitask and forget to log out, creating easy access points for unauthorized users. To prevent this, enable auto-lock after inactivity, use unique credentials, and avoid letting others use your session. Proper logout habits and awareness of your workstation's exposure can drastically reduce the risk of data breaches in clinical environments.
-
HIPAA holds medical assistants directly accountable for protecting electronic health records (EHR/EMR) within their role. It mandates that access be limited to job-relevant tasks, with strict penalties for unauthorized viewing, editing, or sharing of patient data. Assistants must understand the scope of their access rights and avoid viewing information not relevant to their assigned duties. HIPAA also outlines requirements for workstation security, password protection, and patient privacy during digital interactions. Training like the one provided in ACMSO’s certification ensures assistants stay compliant and audit-ready.
-
The best approach combines strong passwords, regular resets, and 2FA (two-factor authentication). Avoid using personal details or repeating passwords across systems. Use password vaults approved by your clinic’s IT policy and ensure credentials are not stored in browser autofill tools. Enable login timeout settings to auto-logout after inactivity. Clinics may also assign role-based access—you should only have the minimum permissions required for your job. Consistently updating and managing passwords reduces exposure from phishing, internal threats, or lost devices.
-
Yes, but only when strict protocols are followed. Remote access must be secured via VPNs, clinic-owned devices, and encrypted platforms. Assistants should never use public Wi-Fi or save login details in personal browsers. Regular audits should be conducted to monitor access logs, and all devices must use antivirus software and endpoint protection. Cloud-based EMRs offer flexibility, but only when paired with well-trained administrative staff who follow security practices—something ACMSO certification programs directly train assistants for.
-
Look for irregular login patterns, such as access during off-hours, or activity from departments unrelated to a patient file. Other red flags include frequent edits to the same chart or changes that don’t match appointment history. Assistants should also be cautious when staff or patients ask for printouts or data outside typical workflows. Use software that tracks access trails—many EMR systems log edits, access times, and user IDs. Being able to recognize and report anomalies is a key part of modern medical admin training.