How to Optimize Your Daily Patient Schedule: Proven CMAA Techniques
Efficient patient scheduling isn’t just about avoiding double bookings—it’s about streamlining patient care, maximizing daily throughput, and boosting satisfaction rates without burning out your team. Medical administrative assistants, especially Certified Medical Administrative Assistants (CMAAs), are the backbone of this process. In clinics, urgent care centers, and specialty offices, the ability to strategically design a daily schedule can reduce no-shows, improve provider utilization, and even increase revenue by up to 15% per day. But achieving that balance requires more than instinct—it demands repeatable systems, digital tools, and front-desk precision.
In this guide, we’ll break down proven, CMAA-endorsed techniques that optimize every minute of your clinic’s calendar. Whether you're managing five providers or just one, these methods apply. From buffer zone logic to intelligent triage spacing, from using integrated EMR schedulers to reducing wait times without overbooking—we’ll cover it all. You’ll also see how the ACMSO CMAA Medical Assistant Certification equips you with practical, system-based scheduling mastery using real-world tools. The result? Smoother patient flow, happier staff, and fewer costly errors. Let’s dive deep into the exact systems used by top-performing CMAAs across the country.
Anatomy of an Efficient Front Desk Schedule
A medical front desk isn’t just where appointments are booked—it’s where clinic efficiency is either set up for success or sabotage. An optimized schedule can cut patient bottlenecks by up to 40%, elevate provider performance, and reduce daily stress across the team. But for that to happen, the CMAA must control not just when patients are seen—but how the flow unfolds throughout the day.
That starts with strategic structure. Smart daily scheduling isn't about cramming slots—it’s about designing intentional blocks of time to accommodate multiple visit types, varying provider tempos, and patient behavior patterns. When structured right, your schedule acts as a living system: adjusting in real time while maintaining predictability and rhythm. Below, we break this down into two critical CMAA techniques that form the backbone of every efficient calendar.
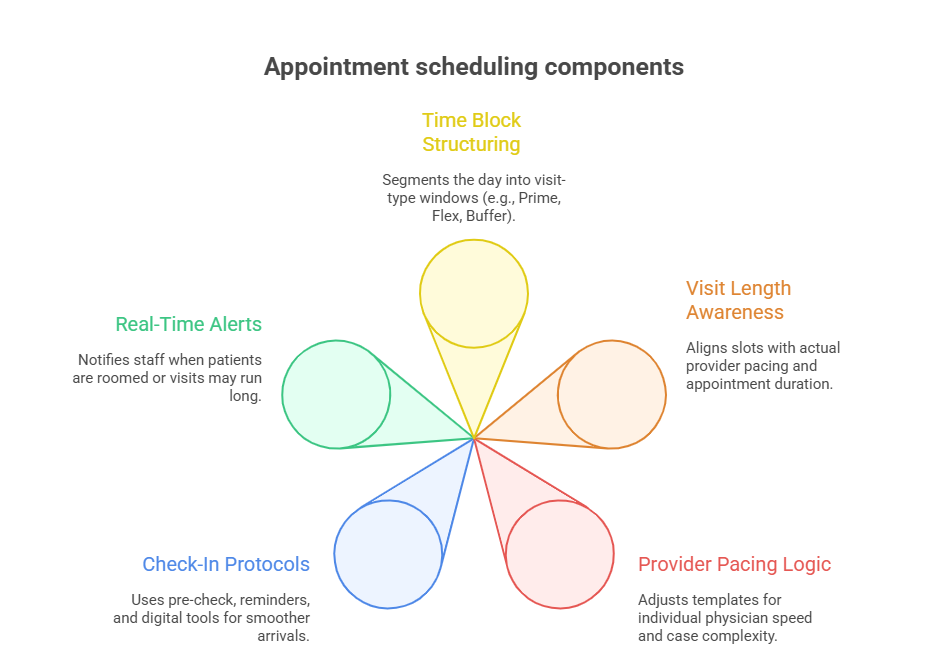
Time Blocks, Visit Types, and Flow
Grouping appointments by clinical category, visit duration, and expected outcome is a foundational tactic for CMAAs. Most high-performing clinics structure their day into segments like:
Morning Prime (8–11 AM): New patient evaluations, post-op checks, or any visit that’s longer than 20 minutes. These require alert providers and uninterrupted focus.
Midday Flex (11 AM–2 PM): Shorter follow-ups, test reviews, and same-day calls. These are fast-moving visits that benefit from back-to-back sequencing.
Afternoon Buffer (2–5 PM): Walk-ins, procedure overflows, or patients with historically lower punctuality. This window must allow flexibility without chaos.
By categorizing visit types into clear time blocks, CMAAs can prevent scheduling chaos before it starts. For example, stacking long consults back-to-back often leads to mid-day burnout. But spacing these with shorter visits maintains flow and supports staff endurance. Additionally, be mindful of provider pacing—some physicians work faster than others, and schedules should reflect those differences.
Using historical data also helps. If patients with specific conditions or age groups routinely arrive late or run long, this insight should directly impact how their appointments are scheduled. A data-informed CMAA schedule is always one step ahead of the day.
High-Impact Check-In Protocols
Front-desk efficiency isn’t just about booking—it’s about preparing for the patient’s arrival before they step in. Top CMAAs deploy pre-visit readiness techniques that streamline check-ins and reduce morning pileups:
Pre-check via text/email (24 hours prior): Patients confirm insurance, upload ID cards, and fill out intake forms remotely.
5-minute arrival windows: Clear signage and automated reminders stress that patients arriving more than 5 minutes late may need to reschedule.
Tablet-based sign-ins: Minimizes paper clutter and allows instant syncing with the EMR.
One high-impact move? Triage alerts sent directly to nurses once a patient checks in. This real-time handoff allows the care team to prep before the patient hits the exam room. Clinics using this model have reported 20–30% faster rooming times and drastically reduced front-desk congestion.
To maintain momentum, front-desk staff should also flag complex cases during check-in. A flagged appointment notifies providers that the upcoming visit may run long, prompting real-time decisions on whether to adjust buffer slots or redistribute duties. Small details like this prevent schedule derailments that compound by late afternoon.
Reducing Wait Times Without Overbooking
The most common trap in medical scheduling is trying to fix delays by squeezing in more appointments. Overbooking doesn’t solve inefficiencies—it multiplies them. Instead, CMAAs trained in optimized flow management use precision-based spacing, walk-in logic, and patient-type stratification to maintain velocity without chaos. Reducing wait times is not about seeing more patients—it’s about seeing the right patients at the right time using the right structure.
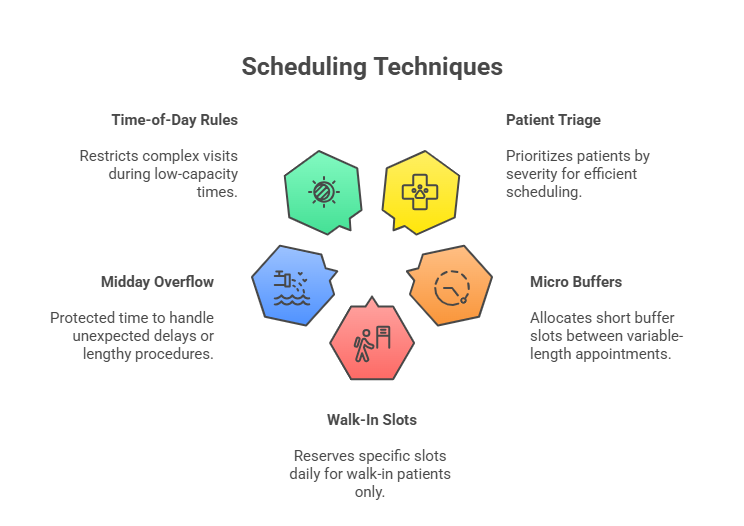
Appointment Spacing and Triage Tools
Every schedule should be built around true visit length, not theoretical slot durations. If a provider averages 18 minutes per follow-up, slotting 15-minute intervals is a setup for backlog. CMAAs should build a “length profile” for each provider and visit type—data that becomes the blueprint for sustainable appointment pacing.
Here’s how to deploy it:
Adjust spacing by service line: Preventive visits and chronic care follow-ups should never share the same time template. Use 20–25-minute spacing for higher-complexity cases, while clustering lower-acuity cases in tighter groupings.
Use triage tools at booking: Have front desk staff ask pre-screening questions to assign a severity level. Use color coding or EMR flags to instantly identify longer-visit needs.
Visual capacity dashboards: Software like AthenaHealth and Kareo allow CMAAs to see live traffic forecasts for the day, helping spot early signs of overload.
The key is building room for variability. Even the best schedule derails if there’s no bandwidth for a delayed patient or surprise walk-in. That’s where buffer logic comes into play.
Using Buffers and Walk-in Logic
Buffer zones aren’t optional—they’re required. The most efficient CMAA-led clinics insert mini-buffers every 3–4 patients, and larger buffers around midday to handle provider debriefs, patient holds, or complex procedures that go long. These buffers function as shock absorbers, preventing small disruptions from cascading into afternoon gridlock.
There are three buffer types CMAAs should master:
Micro buffers (5–10 mins): Inserted after high-variability patients or before double bookings.
Midday reserves: Blocked slots that can be opened same-day for overflows or urgent needs.
End-of-day recovery zones: Optional, but ideal for practices with frequent evening backlog.
Walk-in logic complements buffer zones. Instead of allowing walk-ins to compete with scheduled patients, CMAAs create walk-in only slots, usually 2–3 per provider, per day. These should be clearly marked and reserved until 90 minutes before end-of-day. If unused, they convert back into bookable slots automatically.
The smartest systems also use “time-of-day rules”—for instance, avoid walk-ins during lab changeover hours or provider shift transitions. These nuances let walk-ins serve their purpose (access) without sabotaging flow.
Combined, intelligent spacing and buffer logic reduce average wait time by up to 35% while improving patient experience scores and lowering staff stress.
Automating with Scheduling Software
Manual scheduling is no longer sustainable in modern healthcare. From multi-provider clinics to solo practices, the key to staying efficient lies in automation. Certified Medical Administrative Assistants (CMAAs) are trained to use intelligent scheduling platforms that don’t just book slots—they learn from behavior, predict demand, and fill cancellations in real-time. Leveraging software allows you to reduce errors, streamline patient communication, and keep your team working on schedule 20–40% more consistently.
Integrated EMR Schedulers
An integrated EMR scheduler isn’t just a calendar—it’s the nerve center of clinic logistics. Tools like AdvancedMD, Kareo, or eClinicalWorks allow CMAAs to align appointments with real-time provider availability, resource constraints, and patient history—all from a unified interface. This eliminates the guesswork and prevents time-slot conflicts.
Key features CMAAs should activate:
Provider-specific templates: Assign visit types to specific time blocks based on the provider’s pace and patient load history.
Real-time resource syncing: Ensure that rooms, imaging equipment, or interpreters are available before confirming an appointment.
Smart routing: Send new patients to the provider with the lowest future load or fastest turnaround time, balancing the long-term schedule.
Most advanced schedulers also allow custom rule programming. For example, you can build a rule that prevents back-to-back high-acuity visits or flags when a double-book request violates your clinic’s max-patient-per-hour threshold.
When CMAAs harness these features, they shift from reactive scheduling to predictive, proactive systems that anticipate bottlenecks before they form.
Cancellation Handling & Fill-in Features
No-shows and last-minute cancellations cost clinics thousands of dollars weekly—but smart automation can reclaim that lost time. The best platforms come with cancellation handling engines that act the moment a slot opens.
Here's what CMAAs can set up:
Automated waitlists: When a cancellation occurs, eligible patients from a pre-filtered waitlist are notified by SMS or app alert and can claim the spot instantly. Clinics using this system report 25–35% higher fill rates.
Last-minute opening alerts: Push notifications to same-day patients who may want to come in earlier, reducing empty periods and compressing the day’s schedule.
Patient ranking logic: Sort waitlist patients by urgency, visit type, or reliability score (i.e., no prior no-shows), ensuring the right patient is pulled in.
Cancellation automation doesn’t just preserve productivity—it also sends a strong message to patients that your practice values efficiency and access. And when combined with performance dashboards that show daily open-slot rates and fill velocity, CMAAs can fine-tune scheduling strategies in real time.
Ultimately, automation is not about replacing judgment—it’s about amplifying the CMAA’s decision-making power with tools that keep pace with a high-volume clinical setting.
| Tool Feature | What It Solves |
|---|---|
| Integrated Provider Templates | Builds personalized time-slot templates for each provider based on historical data, patient load, and service complexity. Helps ensure appointment durations match actual clinical time, preventing overbooked slots or underutilized hours. |
| Live Waitlist Fillers | Automatically notifies and schedules pre-filtered patients when cancellations occur. Reduces empty slots due to no-shows and fills gaps in real-time without manual outreach by front-desk staff. |
| Smart Patient Routing | Uses rules-based logic to assign new patients to the most suitable provider based on availability, specialty, and daily volume. Balances clinic workloads and reduces wait time disparities across providers. |
| Cancellation Alerts | Sends real-time SMS, app, or email alerts to patients when an earlier time becomes available. Increases schedule flexibility while improving patient experience and clinic revenue recovery from sudden drops. |
| Visual Capacity Forecasting | Provides CMAAs and managers with at-a-glance dashboards showing peak traffic periods, provider strain, and open slot trends. Enables proactive decision-making before bottlenecks occur. |
Staff Coordination for Smooth Patient Flow
Even the most optimized schedule will collapse if staff coordination fails. Certified Medical Administrative Assistants (CMAAs) play a vital role in aligning front desk operations, clinical intake, and provider availability into one seamless workflow. When done right, patient handoffs happen smoothly, room turnover speeds up, and provider downtime is minimized. The secret isn’t working faster—it’s working in sync.
Intake, Rooming, and Provider Alerts
The intake process is where many clinics lose momentum. Delays in vital signs, form reviews, or room assignments can back up the entire schedule. CMAAs trained in real-time communication systems help streamline this transition by ensuring:
Color-coded status boards show where each patient is in the visit cycle—checked-in, roomed, ready-for-provider, or pending labs.
Immediate rooming alerts are pushed to medical assistants once a patient completes check-in, allowing for faster handoffs.
Provider alert flags notify physicians when the next patient is ready, reducing wait times between consults by up to 30%.
Well-run clinics also assign specific staff to monitor these statuses throughout the day. CMAAs should lead daily morning huddles where provider availability, staff shortages, or walk-in volume projections are discussed and addressed proactively.
Cross-Training Support Staff
Too often, bottlenecks happen simply because roles are siloed. A patient is ready for vitals, but no MA is available. A provider needs a chart pulled, but the front desk is swamped. This is where cross-training becomes a force multiplier.
CMAAs who cross-train support staff unlock three major advantages:
Room turnover flexibility: When medical assistants are trained to handle basic intake or cleaning, rooms can be reset faster during high-volume hours.
Float staff utility: Cross-trained floaters can jump in where needed—front desk, labs, or exam rooms—during peak times or sudden absences.
Break coverage: Scheduled breaks no longer stall patient flow because duties can rotate without gaps in service.
Cross-training also builds team accountability. When every staff member understands adjacent roles, communication improves and errors drop. Clinics that invest in role redundancy report smoother patient journeys, fewer appointment delays, and higher staff satisfaction.
In short, staff coordination is the glue that holds the schedule together. Without it, even the best system will unravel under pressure.
| Role/Function | Coordination Impact |
|---|---|
| CMAA Communication Lead | Serves as the central point of coordination across the front desk, providers, and support staff. Conducts daily morning huddles, highlights anticipated disruptions (e.g., overbooked slots, staff shortages), and ensures alignment before patients arrive. |
| Rooming Staff Alerts | Enables real-time communication between the front desk and medical assistants. Alerts are triggered immediately after patient check-in, allowing rooming staff to prepare and expedite intake processes, cutting transition delays by up to 30%. |
| Color-Coded Patient Status | Tracks the real-time journey of each patient using status labels such as “Checked In,” “Vitals Taken,” “Ready for Provider,” or “Awaiting Lab.” Ensures all team members know exactly where a patient is at any point in the care cycle. |
| Float Staff Deployment | Leverages trained staff who can temporarily fill gaps across departments—whether assisting with intake, room turnover, or document management—during peak hours or unplanned staff absences. |
| Cross-Trained Team Members | Builds internal flexibility by training staff across multiple roles (e.g., front desk, intake, room prep). Reduces workflow disruptions when someone is unavailable, and enhances team resilience during high-demand periods. |
Common Scheduling Mistakes to Eliminate
Efficient scheduling isn’t just about what you do—it’s also about what you stop doing. Certain outdated habits and shortcuts can quietly sabotage the day before it begins. CMAAs trained in system-based scheduling know how to spot and eliminate patterns that lead to delays, no-shows, and provider frustration. Removing these blind spots can immediately improve daily flow and reduce errors by up to 45%.
Manual Confirmations, No Follow-Ups
Relying on manual phone calls to confirm appointments is one of the most common front desk pitfalls. Not only is it time-consuming—it’s also wildly inconsistent. Many patients miss calls, ignore voicemails, or forget what time they booked. Clinics that still depend solely on this method often experience 15–25% higher no-show rates.
To fix this:
Use multi-channel reminders: Deploy SMS, email, and app-based alerts based on patient preferences.
Automate second reminders: Send a follow-up nudge 2 hours before the appointment to improve same-day recall.
Enable easy confirmations: One-click confirmations in texts or apps boost response rates and reduce front-desk workload.
Equally problematic is the failure to follow up on missed appointments. When a patient no-shows, many systems don’t trigger rebooking protocols. CMAAs should create a “missed follow-up” list that is reviewed daily, ensuring high-risk patients are rescheduled promptly.
This proactive recovery step helps retain continuity of care and fills open slots before they go stale.
Double Booking Without Context
Double booking isn’t inherently wrong—it’s about how it’s done. Uninformed double booking causes cascading delays that can derail an entire day. The problem? Many clinics apply a one-size-fits-all approach without factoring in provider speed, patient type, or time-of-day variability.
Smart CMAAs follow these double-booking rules:
Only double book providers with a proven throughput capacity—measured in patients per hour and average visit length.
Use conditional logic: Only double book low-acuity follow-ups (e.g., quick med checks) and avoid pairing two new patients or procedures.
Insert micro-buffers before and after: Never place back-to-back double bookings without room to absorb delays.
More importantly, the scheduler should always visually flag double-booked slots in the EMR or scheduling software. This allows providers and support staff to anticipate volume and adjust pace or priorities as needed.
Mistakes in scheduling are rarely noticed in the moment—they surface as cumulative stress, longer wait times, and patient dissatisfaction. Eliminating these common traps is the first step toward building a bulletproof schedule.
| Mistake | Consequence | What to Do Instead |
|---|---|---|
| Manual Confirmations Only | High no-show rates due to missed calls and lack of real-time sync | Use automated reminders via SMS, email, and app with one-click confirmation options |
| No Follow-Up on No-Shows | Lost revenue, broken care plans, and reduced patient retention | Create daily missed-appointment reports and proactively rebook high-risk patients |
| Unflagged Double Booking | Provider overload, longer wait times, and staff misalignment | Clearly flag double-booked slots and only use for low-acuity, short-duration visits |
| Ignoring Provider Speed Variance | Backlogs caused by mismatched slot durations and clinical pacing | Customize schedules per provider using past performance and visit-type data |
| Stacking Complex Visits Together | Burnout, overtime, and unpredictable patient flow | Alternate long visits with short ones and insert micro-buffers between high-acuity slots |
ACMSO Certification Helps You Master Scheduling Systems
Optimized scheduling isn’t just a front-desk skill—it’s a clinical strategy. Medical scribes trained under the ACMSO CMAA Certification go beyond documentation support. They’re taught how to understand, contribute to, and even manage clinical flow using scheduling logic, patient throughput data, and real-time EMR tools. The result? A workforce that reduces bottlenecks, improves time-to-treatment, and increases billing accuracy—all while boosting provider productivity.
ACMSO’s Practical Modules + Software Demos
Most scribe programs only teach you how to chart. But ACMSO’s curriculum focuses on clinical integration, training scribes to work in sync with schedulers, providers, and front-office teams. Here’s what sets it apart:
Scheduling logic modules: You’ll learn how to read and interpret provider pacing, recognize double-booking red flags, and spot inefficiencies in daily clinic grids.
Flow-sensitive charting: Instead of creating backlog, you'll be trained to chart in sync with provider tempo—cutting charting time by 35–50% while supporting the patient schedule.
Live EMR simulation labs: Get hands-on with actual scheduling tools like Epic, Cerner, or AdvancedMD. These demos cover calendar syncing, smart alerts, and rescheduling workflows.
This hands-on exposure gives you an edge in fast-paced clinics, where scheduling isn’t static—it evolves hour by hour. Scribes with this training are often trusted to flag late-running rooms, communicate time overruns, and adjust visit expectations with precision.
And since medical scribes sit directly at the point-of-care, they become the early warning system for delays. Through ACMSO’s training, you’ll learn how to surface that data upstream to the front desk, ensuring adjustments happen before delays pile up.
Explore the ACMSO Certification
The ACMSO CMAA isn’t just about documentation—it’s about transforming scribes into clinical operations allies. Whether you're working in an urgent care center, surgical practice, or multi-specialty group, this certification equips you to:
Identify inefficient scheduling patterns in real time
Communicate scheduling concerns directly to providers and front desk teams
Integrate EMR alerts and patient flagging tools to support timely care delivery
If you're serious about working at the intersection of clinical efficiency and provider support, this is the training to pursue. Explore the full breakdown of lessons, EMR labs, and real-world clinic scenarios by visiting the ACMSO Medical Scribe Certification course page. Learn how this dual-skill approach not only makes you a better scribe—but a critical asset in every room you step into.
Frequently Asked Questions
-
While both roles interact with the schedule, medical scribes focus on real-time documentation and ensuring the provider’s pace is supported without disruption. Medical assistants, especially certified ones, may handle appointment booking directly. However, scribes with the ACMSO Medical Scribe Certification are trained to monitor room flow, flag delays, and notify the front desk when a schedule is off track. They don’t typically manage bookings, but their visibility into how appointments play out in real time helps the entire care team adapt. This makes scribes valuable for real-time schedule optimization, charting efficiency, and time-to-treatment accuracy.
-
Absolutely. Scribes trained under high-level certifications like ACMSO are taught to chart in sync with provider movement, minimizing delays between patients. By reducing the time a provider spends on documentation, scribes help clinics stay on pace or recover when behind. Moreover, certified scribes are trained to alert staff when delays occur, which allows the front desk or medical assistants to shuffle or reschedule patients more proactively. When the scribe keeps up with real-time flow, the provider is freed up to see patients faster, shortening average visit duration without sacrificing quality.
-
The ACMSO program goes beyond basic charting. It includes practical modules on clinic flow management, integrated EMR systems, and real-time alerts. Trainees learn how to interpret appointment pacing, recognize documentation bottlenecks, and support schedule adherence through real-time flagging. You’ll also use live EMR demos to simulate managing documentation speed based on patient load and time pressure. Unlike programs that train you to react, ACMSO teaches you to anticipate scheduling problems—like patient overload, double booking risks, or overflow without buffers—and help the team adjust before disruptions occur.
-
The ACMSO Medical Scribe Certification includes simulation labs with tools commonly used in real-world clinics. While the specific platform may vary, you’ll get hands-on exposure to:
Epic’s scheduling interface for managing patient loads
Cerner alerts and real-time status flags
AdvancedMD’s calendar and provider pacing view
Waitlist automation and patient recall systems
You’re not just learning to chart—you’re learning to work inside these systems to support the overall scheduling structure. This gives you a direct edge in interviews and prepares you for clinics that expect scribes to understand how charting impacts patient throughput.
-
Clinics today don’t just want scribes—they want scribes who improve clinical efficiency. If you understand how scheduling systems function and how to support real-time flow, you become a far more valuable hire. Hiring managers often look for scribes who can flag delays, communicate patient flow issues, and help keep the provider moving. The ACMSO certification teaches you these skills explicitly. As a result, certified scribes often find more opportunities in fast-paced environments, including urgent care, surgical centers, and large outpatient networks that rely on tight schedules.
-
Yes, but from the clinical support angle. While front desk teams usually rebook patients, scribes certified through ACMSO are taught to spot the clinical implications of cancellations. For instance, if a high-priority patient cancels, you’ll know how to communicate that upstream to suggest a same-day fill-in. Similarly, when a patient’s appointment runs long, scribes can assist in coordinating room use or reassigning provider time. You won’t be the one rebooking—but you’ll ensure the reschedule doesn’t create documentation chaos or patient care delays. That’s a key operational advantage clinics look for.
-
Extremely. Urgent care clinics and ERs run on tight time metrics and unpredictable volume. In these environments, scribes must document fast, adjust to variable pacing, and flag when providers are falling behind. The ACMSO Medical Scribe Certification prepares you for this by simulating fast-paced workflows, buffer logic, and overflow prioritization. You’ll learn how to adjust documentation styles based on acuity and notify teams of backlogs in real time. Scribes with this training are often placed in trauma bays, triage areas, and extended-hours clinics because they support flow under pressure.
Summing Up: Scheduling Mastery
Mastering patient scheduling isn’t just a front-desk task—it’s a clinic-wide performance skill. From reducing wait times to streamlining documentation and anticipating provider delays, the modern scribe plays a powerful role in orchestrating patient flow with precision. With the right training, you’re not just reacting to the schedule—you’re helping shape it.
The ACMSO CMAA Certification empowers you to think like an operations lead, act like a clinical partner, and document with both speed and strategy. You’ll walk into any clinical setting equipped with EMR-driven scheduling logic, charting agility, and a deep understanding of how real-time coordination keeps every appointment on track. If you want to go beyond the clipboard and become the scribe clinics fight to hire, mastering scheduling is your next move.
Quick Poll: What’s the biggest challenge in your clinic’s daily schedule?