Ultimate Guide to Medical Appointment Scheduling Efficiency
In today’s high-volume clinical settings, appointment scheduling efficiency is no longer a nice-to-have — it’s a mission-critical function tied directly to patient retention, revenue integrity, and care quality. When schedules are off, the ripple effects hit every level: longer wait times, missed procedures, burned-out staff, and dissatisfied patients. But when streamlined, scheduling becomes a quiet powerhouse — maximizing every provider’s time, minimizing administrative drag, and ensuring patients get timely access to care.
This guide breaks down the core scheduling strategies, tools, and protocols that separate thriving practices from chaotic ones. Whether you manage a solo provider calendar or coordinate across departments, you’ll gain high-impact insights pulled directly from the ACMSO Medical Scribe Certification training. From real-time calendar control to front-desk scripting and EMR integration, every section is built for tactical execution — not theory. It’s time to turn your scheduling into a precision system.
Why Scheduling Efficiency Matters
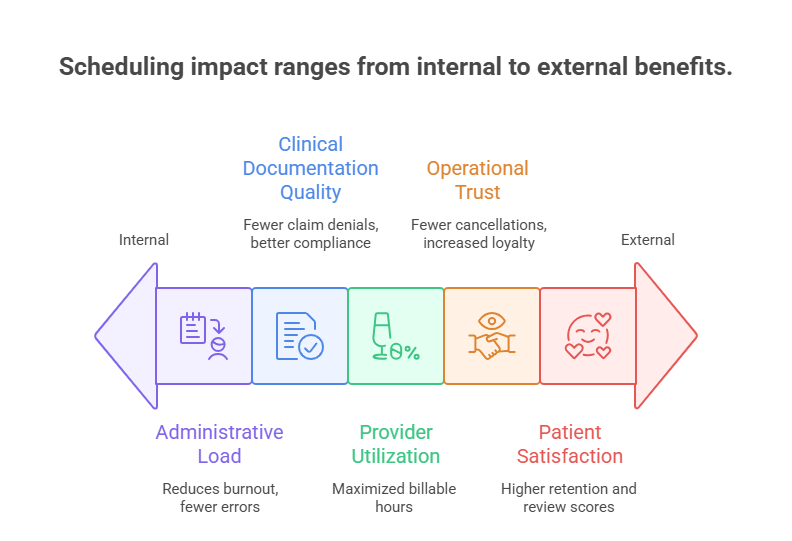
Administrative Load and Patient Satisfaction
A poorly run schedule doesn't just waste time — it compounds stress across the clinical environment. When front-desk teams are stuck reacting to last-minute changes or overbookings, medical administrative burden increases by up to 40%, according to industry audits. This slows check-ins, delays charting, and reduces overall operational efficiency. For the patient, this translates to frustration and longer in-office wait times, which can directly reduce their willingness to return.
Efficient scheduling frees up the front desk to focus on accurate intake, pre-visit verification, and insurance capture — all of which fuel the revenue cycle. Patients are also more likely to perceive the care experience as professional and seamless when appointment times are honored. Studies show that on-time scheduling improves patient satisfaction scores by 28% or more, which impacts not just retention but also provider ratings and reviews on public platforms.
Beyond perception, there’s a trust factor. When schedules run late, patients assume that delays are systemic. This erodes their confidence in the care team’s competence — even if the actual clinical care is excellent. When medical scribes and front-office staff are trained to spot gaps and restructure appointments in real time, that confidence is restored. Well-managed calendars improve both outcomes and loyalty, especially for recurring or specialty care.
Revenue Cycle and Time Blocks
Each empty time slot is a lost revenue opportunity. In many practices, a single missed or misaligned appointment can mean $150–$300 in unreimbursed time, depending on the provider type and specialty. Multiply that by daily inefficiencies, and the financial bleed becomes unsustainable. Scheduling efficiency plugs those leaks and ensures maximum billable utilization of each clinical hour.
By organizing time blocks by visit type, provider availability, and complexity, practices gain control over throughput. New patient consults, follow-ups, and urgent visits should never compete for the same slots. Segmentation also allows for predictive planning: understanding which appointment types are likely to overrun lets schedulers proactively adjust buffers, rather than reactively reschedule.
Tight scheduling also supports better documentation and billing compliance. When visits run on time, scribes can capture real-time notes accurately and completely. That leads to better coding, fewer denials, and higher first-pass claim acceptance rates. Efficient calendars aren’t just about productivity — they’re a critical part of practice profitability.
Techniques for Optimizing Scheduling
Double Booking vs Buffering
Double booking often sounds like a shortcut to efficiency, but without proper safeguards, it backfires. When used indiscriminately, it results in longer wait times, rushed visits, and higher burnout rates. But when applied strategically — such as overlapping quick follow-ups with no-show–prone appointment types — it can boost throughput without sacrificing quality.
Buffering, on the other hand, creates controlled flexibility. By intentionally building 10–15 minute gaps between high-risk or complex appointments, practices can absorb delays without derailing the rest of the day. These buffers also allow space for urgent walk-ins, last-minute changes, or provider charting, which improves documentation accuracy.
The best-performing clinics combine both strategies. They double book only during peak hours, and only with appointment types that are short, predictable, or have high no-show rates. Then they embed small buffers throughout the day for recovery. This model reduces idle time while avoiding traffic jams. It also gives medical scribes space to maintain real-time notes, ensuring billing and compliance accuracy.
ACMSO’s Medical Scribe Certification emphasizes scheduling logic alongside documentation skills, enabling scribes to understand why timing precision matters. A well-informed scribe contributes to more than record-keeping — they become a gatekeeper for throughput and care quality.
Time-of-Day Optimization
Different hours of the day yield different patient behaviors. Morning slots typically attract older adults and high-adherence patients, while late afternoon slots see more cancellations and no-shows. By analyzing historical attendance patterns, practices can assign high-risk appointment types (e.g., new consults, chronic care) to peak commitment windows.
Additionally, aligning appointment types to the provider’s performance rhythm improves flow. Some clinicians are more efficient early in the day, while others prefer to batch procedures after lunch. Matching schedule intensity to the provider’s pace improves both clinical care and morale.
Smart schedulers also front-load complex or high-revenue cases, ensuring that if delays occur, they don’t affect the most financially valuable visits. Time-of-day optimization isn’t just about convenience — it’s about maximizing efficiency and revenue per hour.
Many EMR-integrated tools now offer predictive scheduling that recommends ideal slot placements based on patient history, visit type, and provider habits. When front-office staff and scribes are trained to interpret these insights, it leads to better planning and fewer day-of disruptions. Time-of-day scheduling is one of the least used but most powerful levers in appointment optimization.
| Technique | Description | Strategic Outcome |
|---|---|---|
| Double Booking | Layering quick visits in high no-show windows | Increased capacity with minimal overload risk |
| Buffering | Adding time between visits for flexibility | Reduced delay chain and improved pacing |
| Time-of-Day Optimization | Aligning appointment types to patient behaviors | Fewer no-shows, improved patient readiness |
| Slot Segmentation | Grouping visits by complexity or urgency | More predictable visit lengths |
| Data-Driven Patterns | Using past trends to predict best slot usage | Higher efficiency with fewer disruptions |
Digital Tools and Scheduling Software
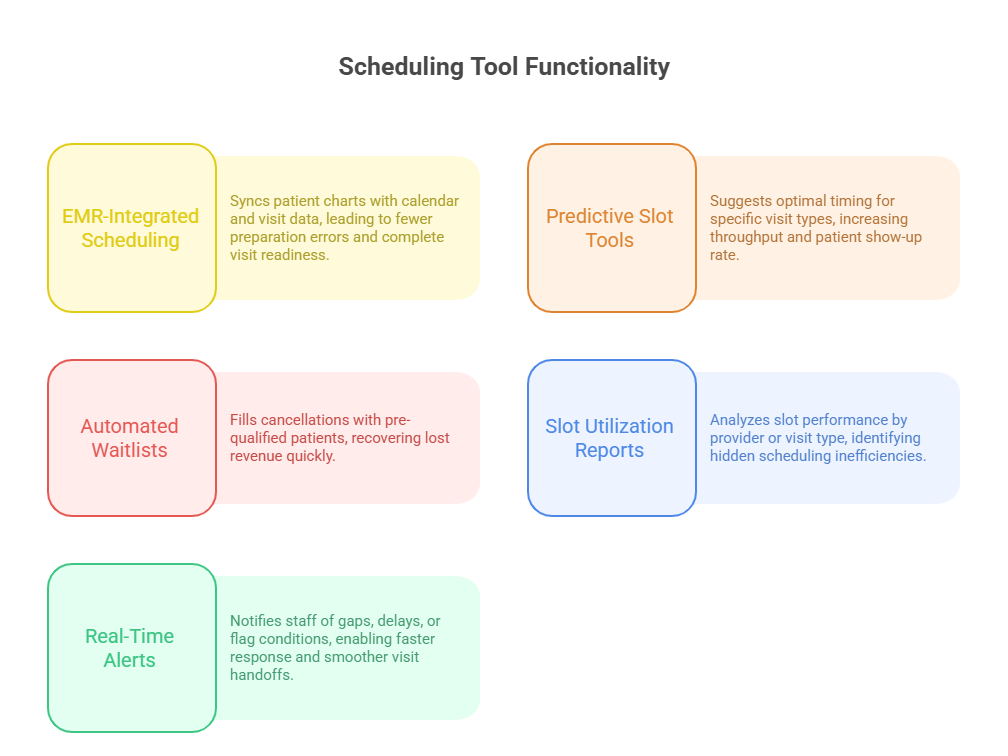
EMR-Integrated Systems
EMR-integrated scheduling platforms do more than book slots—they create real-time sync between clinical documentation, patient intake, and billing. When scheduling lives inside the same system as the patient’s chart, front-desk teams can instantly verify visit history, provider preferences, and insurance eligibility before confirming appointments. This eliminates unnecessary callbacks and prevents costly mismatches.
Integrated systems also provide appointment-specific prep cues, such as required labs, imaging, or pre-visit forms. These prompts increase patient readiness and reduce same-day cancellations due to incomplete prerequisites. When medical scribes are trained to interact with EMR scheduling logic, they help ensure visit prep aligns with documentation goals.
Practices using fully integrated EMR scheduling tools report a 15–25% drop in no-shows and smoother billing cycles due to complete visit documentation at the point of care. EMR alerts can also flag high-risk patients or patterns, like repeated late arrivals, which help teams preempt disruptions.
For example, ACMSO’s Medical Scribe Certification trains scribes to use these systems not only to observe schedules but also to help coordinate chart readiness, patient flags, and provider preferences in real time. The result is tighter care delivery and fewer surprises in the room.
Analytics for Slot Utilization
Most practices think their schedules are optimized—until they analyze the data. Slot utilization reports reveal the hidden inefficiencies in every day: appointment types that overrun, providers whose schedules bottleneck, or times where idle blocks waste billable hours. Scheduling analytics turn these patterns into actionable changes.
For instance, if a report shows that 11:00 AM slots often start late, it could mean earlier patients are receiving unplanned services. Adjusting buffers or restructuring visit types in those windows can resolve the delay. Similarly, if cancellations peak on Fridays, automated waitlist features can dynamically fill gaps with real-time patient outreach.
Modern tools use machine learning to recommend ideal block structures, flag overuse of double-booking, and optimize staff assignment. These platforms do more than show what happened — they forecast how to improve. For a busy clinic, this means recovering 2–4 hours of productive time per week, simply by realigning the calendar with data.
When scribes and schedulers know how to read these analytics, it creates a feedback loop between operations and care delivery. Everyone’s time becomes more valuable. Tools alone don’t drive efficiency — trained professionals with the right insights do.
Staff Training for Front-Desk Efficiency
Scripted Responses & Conflict Handling
Front-desk teams often serve as the first and final point of contact — and every interaction can shape the patient’s perception of care. That’s why scripted responses for common scheduling scenarios (e.g., running late, rescheduling, new patient onboarding) are essential. They reduce hesitation, create consistency, and allow teams to handle friction with confidence.
For example, instead of vague apologies for delays, a scripted response like “Thank you for your patience — your provider is finishing with a patient and we’ll get you in shortly” manages expectations while preserving trust. Training staff to use these scripts naturally ensures smoother exchanges, even during peak-hour tension.
Conflict handling is equally crucial. When two patients show up for a double-booked slot or someone insists on being seen immediately, untrained staff may panic or escalate. But with roleplay-based training, teams can de-escalate quickly, redirect effectively, and maintain schedule flow without creating bottlenecks.
This isn’t just about politeness — it’s about operational stability. Front-desk staff trained in structured scripts and de-escalation techniques can preserve clinic rhythm, minimize fallout, and protect patient experience even in high-stress moments.
Real-Time Adjustments & Waitlist Use
No schedule is perfect by 9 a.m.—appointments get canceled, patients arrive late, and emergencies arise. That’s where real-time calendar adjustments become the make-or-break skill for front-desk teams. Staff should be trained not just to identify gaps but to fill them proactively using tools like dynamic waitlists and auto-text rescheduling.
For instance, if a 2:00 PM slot opens and a same-day patient prefers afternoons, a quick waitlist check and outbound call or text can turn a hole into a productive visit. Automated waitlist features can even scan cancellations and trigger alerts based on match criteria — all staff have to do is approve the replacement.
Effective real-time scheduling also requires cross-role communication. Front-desk teams should notify scribes and nurses of late changes to avoid prep delays or incomplete charting. Without this coordination, schedule changes become liabilities instead of opportunities.
| Training Focus | Skill Taught | Result in Scheduling |
|---|---|---|
| Scripted Responses | Professional communication under stress | Defuses conflict, keeps patients informed |
| Conflict Handling | Techniques to manage double-bookings or late arrivals | Preserves schedule flow |
| Real-Time Adjustments | Filling gaps and adjusting slots dynamically | Maximizes calendar use |
| Waitlist Utilization | Proactive patient outreach for open slots | Reduces no-show impact |
| Cross-Team Coordination | Front desk, scribe, nurse, and provider communication | Fewer breakdowns and missed updates |
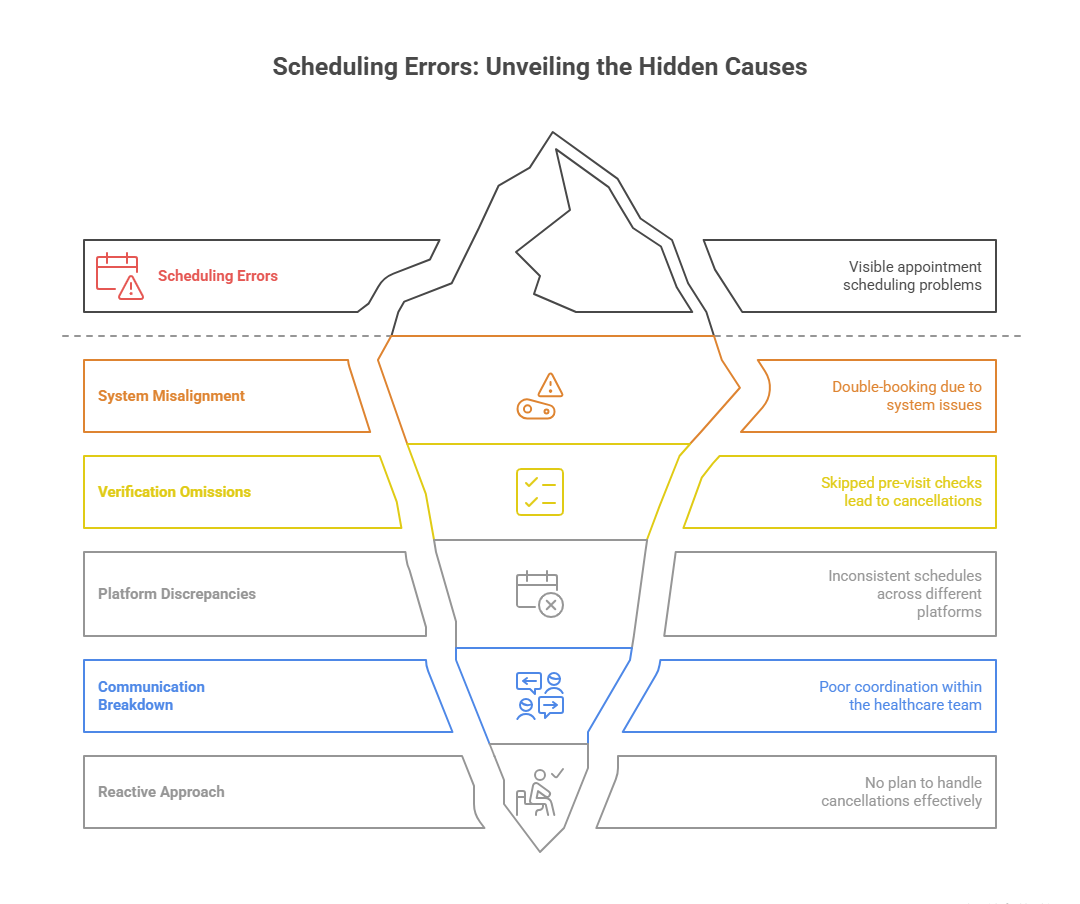
Errors That Undermine Scheduling Flow
Overlaps, No Pre-Visit Checks, Missed Updates
One of the most damaging errors in appointment flow is accidental schedule overlap. This typically occurs when multiple staff members book simultaneously or when recurring appointments auto-populate without flagging conflicts. The result? Two patients, one room, and a stressed-out provider. Even a 5-minute delay can snowball into a 30-minute backlog.
Another common issue is skipping pre-visit checks. When insurance status, referral requirements, or lab results aren’t confirmed in advance, the provider may have to cancel or delay the visit. That wastes time for everyone involved. Training staff and scribes to perform pre-check protocols dramatically reduces same-day disruptions.
Missed schedule updates — especially for last-minute provider time-offs or adjusted clinic hours — are another silent disruptor. When calendars aren't synced across platforms or staff, patients show up for nonexistent visits, and providers lose trust in the system. Calendar visibility and centralized update protocols are essential.
Even the best tools can't compensate for poor execution. Practices must review calendar errors weekly to spot patterns and retrain as needed. Prevention starts with process, not just software.
Lack of Communication Protocols
Even a perfectly designed schedule falls apart without tight internal communication. When front-desk teams, scribes, nurses, and providers operate in silos, appointment flow suffers. If a patient arrives late and no one informs the scribe or provider, valuable minutes are lost realigning prep and notes.
The most efficient practices follow real-time communication protocols. These include tagged notes in EMRs, internal instant messaging systems, or even walkie tools for high-volume clinics. Everyone on the care team should be notified instantly when a visit changes — whether it’s a delay, a no-show, or an added urgent slot.
Another failure point is in handoff communication. If a provider asks for a same-day follow-up and no one relays it to scheduling, the opportunity vanishes. Scribes can support this by flagging follow-up requests in real time and coordinating with the front desk.
The ACMSO Medical Scribe Certification emphasizes cross-role awareness, so scribes become an anchor for coordination — not just documentation. Without protocolized communication, schedule flow becomes reactive instead of intentional, and every efficiency gain is lost to breakdowns in clarity.
ACMSO Training on Scheduling Systems
Workflow Training, Chart Prep, Intake Coordination
The ACMSO Medical Scribe Certification doesn’t stop at documentation — it delivers comprehensive, applied training on how scribes support and enhance scheduling workflows. That includes everything from pre-visit chart prep to coordinating intake protocols and confirming provider-specific slot preferences.
Scribes trained under ACMSO learn how to anticipate workflow friction points: Which appointment types tend to overrun? When do providers need extra buffer time for complex cases? How do referral types influence chart preparation time? These details aren’t random — they’re part of schedule-aware charting and prep that streamlines patient flow and ensures nothing is missed.
Students are also taught how to collaborate with the front desk to confirm lab results, imaging, or specialty referrals before the patient arrives. This coordination closes common gaps that otherwise lead to rescheduling or incomplete visits.
More importantly, scribes are trained to flag prep errors in real time — such as missing intake notes, unsigned consents, or insurance verification mismatches. This proactive role minimizes delays and makes the scribe a key operational partner, not just a passive recorder.
By integrating workflow logic into documentation, ACMSO-trained scribes become a bridge between scheduling precision and clinical accuracy, helping every minute count.
Train Your Team with ACMSO’s Scheduling-Focused Program
For practices looking to tighten their scheduling operations from the inside out, enrolling staff in the ACMSO Medical Scribe Certification program is a high-leverage move. The curriculum includes targeted modules on scheduling systems, real-time workflow adjustments, and chart-readiness coordination — all built around actual practice demands, not generic theory.
Unlike other scribe programs that isolate documentation from clinic flow, ACMSO trains scribes to operate as extensions of the care team. This means understanding the why behind the when — not just recording what’s said, but recognizing the operational context in which care happens.
Students gain exposure to common scheduling platforms (including EMR-integrated tools), roleplay scenarios for intake coordination, and checklists for real-time schedule validation. Every tool taught is mapped to improved patient flow, shorter wait times, and tighter administrative control.
What sets this certification apart is its focus on hands-on efficiency training, designed to reduce the daily chaos of scheduling errors, communication lags, and prep mismatches. Clinics with ACMSO-trained scribes report smoother calendar execution, faster visit turnover, and better morale across both front- and back-office teams.
Whether you’re upskilling current staff or building a precision-driven workforce from scratch, ACMSO’s certification delivers clinic-ready results from day one.
Frequently Asked Questions
-
Efficient medical scheduling ensures that every appointment slot is used to its maximum potential. Without it, clinics experience delays, provider idle time, and reduced patient throughput. When schedules are optimized, clinics can see more patients, reduce waiting room congestion, and minimize stress for staff. It also improves clinical documentation because scribes and providers operate in a predictable rhythm. This consistency leads to better outcomes and higher revenue per clinical hour. Efficient scheduling also directly affects patient satisfaction, as delays or reschedules often lead to dissatisfaction and negative reviews. Simply put, scheduling is the engine of operational efficiency in modern healthcare.
-
The ACMSO Medical Scribe Certification includes real-world training on how scribes can actively support appointment flow. It covers chart preparation, intake coordination, and communication protocols that minimize same-day surprises. Scribes learn how to flag delays, collaborate with front-desk staff, and ensure patient data is complete before the visit starts. They also understand how appointment types impact provider timing. Unlike basic scribe programs, ACMSO’s course is designed to make scribes integral to operational efficiency. They’re not just documentation aides—they’re real-time workflow partners who contribute to on-time scheduling, reduced errors, and faster turnover.
-
Several common mistakes disrupt scheduling flow. These include overlapping appointments, failure to verify insurance or labs before the visit, and lack of communication when the schedule changes. If a provider’s availability shifts and the team isn’t informed, it results in patients arriving for nonexistent appointments. No-show management is also a critical weak point—without automated follow-ups or waitlists, practices lose revenue and waste provider time. Another often-overlooked factor is not segmenting appointment types, which creates uneven visit durations and backlogs. Effective scheduling requires both tools and training to avoid these pitfalls and maintain control over clinic time.
-
No. While digital tools enhance efficiency, they cannot fully replace the critical thinking and context awareness that human schedulers bring. Algorithms don’t always account for provider habits, patient preferences, or sudden changes like cancellations or urgent add-ons. Tools like EMR-integrated scheduling and predictive slot utilization reports work best when operated by trained staff who can interpret and act on insights. That’s why ACMSO trains medical scribes not just to observe scheduling patterns but to support decision-making. Digital tools are most powerful when paired with knowledgeable staff who know how to flex the system in real time.
-
Scribes serve as real-time observers of the clinical schedule. They track whether visits are starting and ending on time, flag bottlenecks, and identify missing intake or documentation elements before they cause delays. Trained scribes can also alert the front desk about extended visits, coordinate with nurses on prep, and ensure the provider stays informed about any change in patient arrival. Through chart readiness, communication, and timing awareness, scribes become a second set of operational eyes that keep the schedule moving. ACMSO’s training emphasizes this multi-functional support as part of its core curriculum.
-
The ACMSO Medical Scribe Certification teaches scheduling fundamentals such as time-blocking by visit type, buffer slot logic, and waitlist strategies. It also includes hands-on exposure to EMR scheduling systems, intake flow coordination, and real-time rescheduling practices. Scribes learn to differentiate between visit types (e.g., follow-up vs new consult), identify high-risk time slots, and prepare charts based on timing logic. This training helps them support not just documentation but clinic throughput as a whole. The course also covers cross-role communication, so scribes can align with front-desk staff when appointments shift unexpectedly.
-
Double-booking involves assigning two patients to overlapping time slots, often to account for potential no-shows or fast-visit types. Buffering, on the other hand, means building intentional gaps between appointments to absorb delays. Both strategies serve different purposes. Double-booking improves utilization but carries a risk of congestion if both patients arrive. Buffering reduces that risk but may lead to underused time if not optimized. The best practices often combine both techniques—using data-driven logic to determine when to double and when to buffer. ACMSO’s program trains staff to understand and support these approaches with clarity.
The Takeaway
Medical appointment scheduling is no longer a background task — it’s a high-impact operational discipline that shapes patient experience, staff performance, and financial outcomes. From time-blocking and EMR integration to real-time adjustments and communication protocols, efficient scheduling is built on strategy, not guesswork. The clinics that thrive are those that treat scheduling as a precision process, not just a calendar exercise.
The ACMSO Medical Scribe Certification empowers scribes to step beyond passive documentation and become active contributors to appointment flow, prep accuracy, and system-wide coordination. Whether you're optimizing one provider’s day or a multi-site operation, this training ensures your staff knows how to keep every minute productive. In a healthcare environment where time is the scarcest resource, efficiency isn't optional — it’s a competitive edge.
| Quick Poll: What’s Your Biggest Scheduling Challenge? | |
|---|---|
| Thanks for submitting your answer! | |