Real-Life Success Stories from Certified Medical Administrative Assistants
In 2026, the strongest Certified Medical Administrative Assistants (CMAAs) are not just “helping the clinic run.” They are quietly fixing the exact problems that drain revenue, spike stress, and push patients away: broken intake, scheduling chaos, incomplete documentation, preventable denials, and provider sign off delays. The real success stories are not feel good quotes. They are repeatable playbooks backed by artifacts you can show in interviews: KPI improvements, cleaner workflows, fewer fires, and better patient experiences. Here are real world style success stories you can copy, even if you are starting from zero.
1) Success Story 1: From “Front Desk Chaos” to a Calm, Fast Patient Flow That Patients Feel
A newly certified CMAA walked into a clinic where mornings were a predictable disaster: long lines, angry patients, and staff blaming each other. The hidden root cause was not “too many patients.” It was undefined intake and inconsistent handoffs. She rebuilt flow like a system.
First, she standardized the first two minutes. Every patient got the same intake sequence: ID and insurance capture, confirmation of preferred contact method, and a one line visit goal. She used scripting principles from the telephone etiquette guide and strengthened patient trust with skills from active listening scenarios. Patients stopped repeating themselves because the clinic stopped asking different questions every time.
Next, she mapped bottlenecks using the framework behind the interactive job demand by specialty report and turned it into a daily “flow board” for the team. Each visit type had a target time range. Anything outside that range triggered a quick note: missing forms, late arrivals, room delay, or provider running behind. This turned complaints into data.
Her proof artifact was simple and powerful: a weekly check in time log, plus a list of the top three causes of delay. Within weeks, the team stopped guessing. They started fixing. This is the kind of outcome driven work highlighted in the CMAA efficiency research and reinforced in the 2026 CMAA insights.
The result was not just “better operations.” Patients felt respected. Providers stopped starting visits already irritated. And leadership saw fewer escalations. That is a CMAA success story with teeth.
2) Success Story 2: The CMAA Who Cut Denials by Owning Eligibility, Prior Auth, and “Preventable Errors”
In many clinics, denials feel like a billing problem. In reality, most preventable denials start earlier: eligibility not confirmed, missing documentation, wrong referral pathway, or a prior auth packet that looks incomplete. A certified CMAA turned denial pain into a win by building a front end “revenue protection layer.”
She started by learning the language. Not coding language, but payer friction language. She used the clarity approach from medical billing explained for admin assistants and documented three denial patterns: coverage inactive, missing referral, and missing medical necessity details. Then she tied each denial pattern to a single prevention step.
Her biggest move was timing. She enforced a rule: eligibility verification happens before the visit window, not at check in. That single shift reduced surprise cancellations and reduced patient anger. She supported it with an internal checklist and a daily dashboard inspired by the systems mindset in medical office automation opportunities.
Then she fixed prior auth submissions with a packet template. Instead of sending whatever the provider happened to write, she standardized the packet: required documents list, visit summary snippet, and clear patient identifiers. When something was missing, she did not “push it through.” She escalated fast with a specific ask. This is the difference between being busy and being effective.
Her proof artifact was a denial reason tracker and a first pass approval rate report. Leadership finally saw the clinic’s preventable loss points. This outcome driven thinking aligns with the skill sets described in future proof CMAA career skills and the broader admin transformation in the virtual administration remote work guide.
The “success” here was not just fewer denials. It was trust. Billing trusted admin. Providers trusted the process. Patients trusted the clinic because fewer surprises happened.
3) Success Story 3: The CMAA Who Became the “Clinic Operating System” by Standardizing Communication
One certified CMAA did not start with automation. She started with language. In her clinic, patients were calling multiple times because answers were inconsistent. One staff member said “call billing.” Another said “we will call you.” Patients heard uncertainty and assumed neglect. That is how trust dies.
She rebuilt communication using three assets:
A call categorization list with “what to say” scripts
A callback promise rule with a clear timeframe
A documentation habit that made the next staff member instantly understand the situation
Her communication style was trained using the telephone etiquette examples and empathy mechanics from active listening training. When callers were upset, she used a predictable structure: confirm the problem, confirm the next step, confirm the timeframe, confirm who owns it. That structure sounds simple, but it is rare. It removes uncertainty, which is what patients actually fear.
Then she eliminated internal confusion by standardizing how messages were routed. If the message required a provider, it was labeled with the minimum required context. If it was administrative, it stayed in the admin lane. This prevented providers from drowning in non clinical tasks and aligned with the productivity patterns described in healthcare admin efficiency insights.
Her proof artifact was a call reason report and a reduction in repeat calls. She also kept a short escalation log showing what triggered escalations and how they were resolved. This is the kind of operational clarity that shows up in the CMAA efficiency research and connects directly to medical office automation strategies.
Her career win was not luck. It was visibility. Leadership finally saw that communication is a system, and she built it.
4) Success Story 4: The Remote CMAA Who Proved Impact Without Being “In the Building”
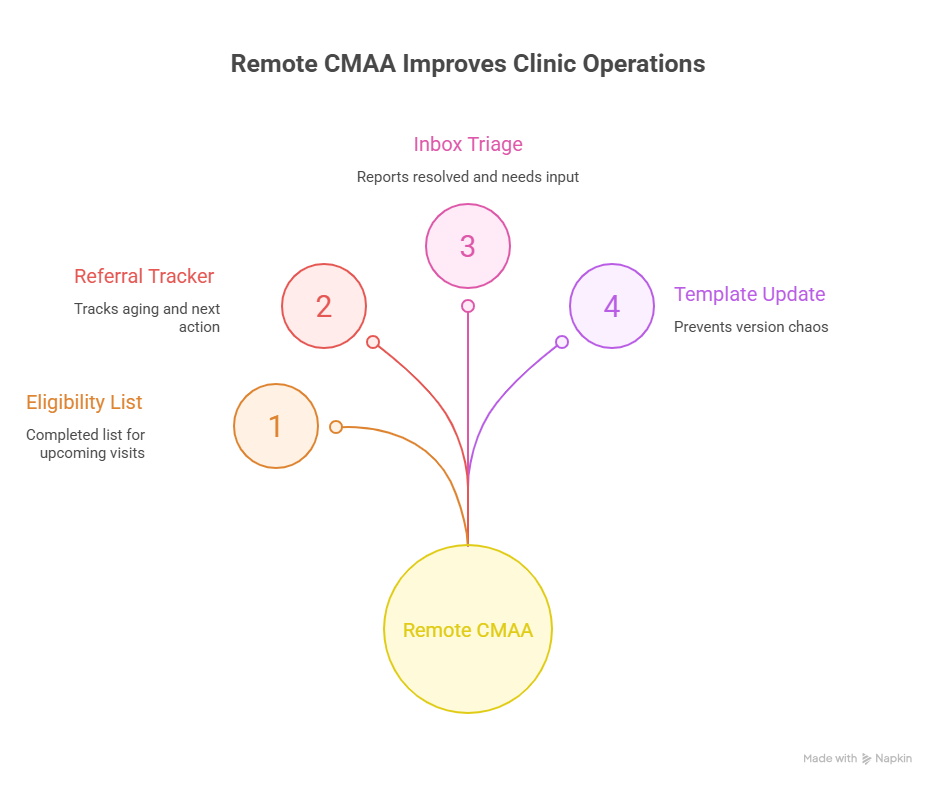
Remote work in administration is no longer a novelty in 2026. It is a competitive advantage when done correctly, and the best remote CMAAs do not “work from home.” They run tightly defined workflows with measurable outputs. A certified CMAA used remote work to become indispensable by owning tasks that are perfect for deep focus: eligibility verification, referral coordination, prior auth prep, message triage, and template maintenance.
She followed the operational patterns in the virtual administration transformation guide and built daily deliverables that made performance undeniable:
A completed eligibility list for upcoming visits
A referral tracker with aging and next action
An inbox triage report with what was resolved and what needs provider input
A template update log that prevented “version chaos”
Her clinic had suffered from template sprawl where staff used outdated forms and inconsistent phrasing. She fixed it with version naming rules and a single template index. That is not glamorous, but it prevents compliance issues and reduces documentation rework. It also overlaps with the systems mindset in EMR software terms and workflows and the broader infrastructure in patient management system guidance.
Her proof artifact was simple: weekly output summaries and a before after comparison of unresolved inbox volume. When leadership can see your output in a clean weekly format, remote work stops being “trust based.” It becomes performance based.
That is the remote CMAA success story: fewer interruptions, more system building, clearer results, and higher trust.
5) Success Story 5: The CMAA Who Used Certification to Negotiate Better Pay, Better Scope, and a Real Career Path
Many CMAAs get stuck because they cannot articulate what they do in business language. They say “I handle front desk” or “I do scheduling.” That language is small, so the pay stays small. One certified CMAA reframed her role and moved up by speaking the clinic’s language: throughput, revenue integrity, risk reduction, and patient retention.
She built her case using internal data, plus market signals from the annual CMAA salary report. Instead of asking for a raise based on effort, she asked based on impact. She presented three wins:
Reduced no shows with confirmation scripts and scheduling rules
Reduced preventable denials by tightening eligibility timing
Reduced provider message overload by using structured triage
She also positioned herself for leadership by creating training assets for new hires and documenting the top workflows. This aligns with what employers want in the emerging CMAA skills roadmap and the broader hiring priorities described in the job demand by specialty report.
Her negotiation was not aggressive. It was clean. She said: “Here are the outcomes, here is the proof, here is how I will scale it across the team.” She offered a next quarter target plan inspired by the outcomes thinking in medical office automation trends. She got a scope upgrade and compensation adjustment because she made the decision easy.
The key insight is this: certification helps, but outcome proof closes the deal.
6) FAQs
-
Start with one tracker that you can update in under five minutes daily. Pick a pain point that causes visible stress, like callbacks, no shows, or referral delays. Track it in a simple table: date, volume, outcome, and reason tags. Use language from patient flow management so your categories match real operations, then connect your improvements to clinic priorities in the 2026 CMAA insights. Proof artifacts work because they shift your value from “trust me” to “here is the impact.”
-
Fix one workflow that touches every patient: check in. Standardize intake questions, create a micro checklist for ID and insurance capture, and build a scheduling decision tree for common appointment types. Pair your communication with the scripts in the telephone etiquette guide and the empathy pattern in active listening scenarios. Track average check in time and the top delay reasons. A small win here creates immediate patient relief and staff trust.
-
Make delays visible and categorized. When the team can see delay reasons as data, blame becomes problem solving. Use a simple daily log tied to visit types and handoffs, then connect your improvements to operational best practices in medical office automation. When you bring proof, you shift the conversation from “who messed up” to “what is the bottleneck.” That shift protects your reputation and makes leadership see you as an operator, not a scapegoat.
-
Employers want CMAAs who can run systems, not just tasks. The highest leverage skills are patient flow management, communication under pressure, eligibility and prior auth coordination, inbox triage discipline, and template standardization. You can map these to the priorities in future proof CMAA skills and the operational trends in healthcare administration insights. If you can also speak clearly about EMR workflows using the EMR software walkthroughs, you become instantly easier to hire.
-
Revenue is protected upstream. Eligibility timing, referral completeness, prior auth packet quality, and documentation consistency prevent denials and reduce rework. Learn the basics through medical billing explained, then build a denial reason tag list and link each tag to a prevention step. Even small reductions in preventable denials compound because they save staff time, reduce patient frustration, and speed cash flow.
-
Make your work visible through outputs, not presence. Deliver daily or weekly summaries: eligibility completed, referrals progressed, inbox items resolved, and templates updated. Follow workflow patterns from virtual medical administration and use structure from patient management systems. Visibility reduces doubt. Output builds trust. That is how remote CMAAs become more secure, not less.
-
Bring outcomes, proof, and a forward plan. Use market context from the annual CMAA salary report, then show your local impact with artifacts: time saved, no shows reduced, denials prevented, or escalations lowered. End with a scaling plan aligned to clinic priorities using ideas from medical office automation trends. You are not asking for a favor. You are presenting an ROI case.