Medical Office Telephone Etiquette: Interactive Dictionary & Examples
In today’s healthcare environment, telephone etiquette in medical offices isn’t just about courtesy—it’s a cornerstone of operational excellence. Patients’ first impressions often stem from these interactions, shaping trust in your practice. A single misstep on a call can trigger compliance risks, lost appointments, or even reputational damage. Medical staff must understand that each phone conversation—whether it’s a routine appointment or delivering sensitive results—represents an opportunity to reinforce the office’s professionalism and compliance.
Proper telephone etiquette combines technical accuracy with human-centric communication. From verifying identities while adhering to HIPAA regulations, to demonstrating empathy with stressed patients, phone interactions require precision and emotional intelligence. Each call is a reflection of your team’s competence and commitment to patient care. This article delivers a value-dense guide, filled with actionable insights, a practical terminology dictionary, real-life scripts, and compliance tips to empower medical professionals with the skills and confidence to handle every phone call with clarity, empathy, and legal compliance.
The Essentials of Medical Office Telephone Etiquette
Why Professionalism on the Phone Matters
In medical offices, professionalism isn’t optional—it’s essential. The tone and clarity of every phone call directly impact patient trust. When staff answer calls with confidence and empathy, patients are more likely to follow instructions and feel valued. Poor etiquette can drive dissatisfaction, leading to missed appointments and negative reviews. Compliance risks also escalate when calls lack proper documentation or privacy protocols. Even small missteps, like improper verification of a patient’s identity, can breach HIPAA rules, exposing your practice to liability.
Professionalism on the phone requires more than a friendly voice. Staff must demonstrate active listening, repeat critical details to confirm understanding, and provide clear next steps. For example, when scheduling a complex procedure, summarizing the discussion before ending the call ensures both compliance and patient confidence.
Key Principles of Effective Medical Calls
A structured approach to every call maximizes clarity and minimizes errors. First, establish the caller’s identity and purpose with concise, courteous questions. Use a calm, measured tone to foster trust. Next, apply active listening techniques: paraphrase, ask clarifying questions, and summarize the caller’s key points. Confidentiality is paramount. Avoid using patient names or sensitive details unless necessary, especially in public or open office spaces.
Respect and empathy are essential. For instance, if a patient is distressed about lab results, acknowledge their emotions before providing information. Use tone modulation to adjust your voice—warm for routine inquiries, calm and firm for escalations. Closing each call with a recap of actions and clear follow-up instructions ensures patients leave the call informed and reassured.
The Role of Compliance and Legal Requirements
Medical office calls must align with HIPAA and state regulations to protect patient privacy and maintain operational integrity. Staff must verify the caller’s identity before sharing any protected health information. For instance, requesting the caller’s full name, date of birth, and medical record number prevents unauthorized disclosure. Calls should be conducted in private or with confidentiality measures, like using headsets or designated call areas.
Documentation is another compliance pillar. Every call should be logged with the date, time, caller’s identity, reason for the call, and any information shared. Failure to document can result in compliance gaps and legal exposure. Training in relevant regulations, including state-specific laws like California’s Confidentiality of Medical Information Act (CMIA), equips staff to handle calls confidently. In cases of escalations or sensitive issues, staff should follow established protocols, including immediate notification of supervisors or legal advisors.
| Poll: What is the most important aspect of Medical Office Telephone Etiquette? | |
|---|---|
| Clear Communication | |
| Compliance with HIPAA | |
| Empathy and Tone | |
The Interactive Dictionary of Telephone Etiquette Terms
Foundational Terms to Master
Active Listening: This means focusing fully on the caller, absorbing not just words but tone and intent. For instance, if a patient says they’re anxious about results, repeating their concern and offering reassurance demonstrates attentiveness.
Call Screening: Identifying the purpose of the call before transferring or responding. For example, asking, “May I know what this call is regarding?” allows staff to prepare appropriate responses or route the call to the right department.
Patient Verification: Essential for HIPAA compliance. This includes requesting the patient’s full name, date of birth, and sometimes a unique identifier before discussing sensitive information.
Hold Protocols: Politely inform the caller when placing them on hold, stating the reason and expected wait time. For example, “I’ll place you on a brief hold while I access your file—this will take about a minute.”
Clear Communication: Use plain language, avoid jargon, and speak slowly enough to ensure understanding, especially for older patients or those with language barriers.
Each of these terms reinforces professionalism and compliance. Proper use of these foundational terms fosters patient trust and ensures regulatory alignment, reducing the risk of miscommunication and errors.
Advanced Etiquette and Professional Jargon
Escalation Protocols: When a caller’s issue exceeds the staff member’s authority, protocols dictate the steps to involve supervisors or clinical staff. A sample script: “I understand your concern, and I’ll connect you with our nurse supervisor for assistance.”
Service Recovery: Techniques for turning negative experiences into positive ones. For example, if a patient was upset about a scheduling error, a staff member might say, “I’m sorry for the inconvenience. Let’s work together to find the earliest available appointment.”
Tone Modulation: Adjusting vocal tone to suit the situation. A softer, calming voice for distressed patients; a confident, firm tone for escalations. This helps de-escalate tension and project competence.
Information Filtering: Avoid overloading the caller with details. Prioritize the most relevant facts and offer to provide more information if needed.
Call Logging: Accurate documentation of each call’s content ensures compliance and continuity of care. A sample note: “5/29, 2:30 PM – Patient requested refill for hypertension meds. Verified DOB and MRN. Call completed, follow-up set for pharmacy call.”
| Term | Definition | Example/Action |
|---|---|---|
| Active Listening | Focusing fully on the caller, absorbing not just words but tone and intent. | Repeating the caller’s concerns, offering reassurance. |
| Call Screening | Identifying the purpose of the call before transferring or responding. | Asking, “May I know what this call is regarding?” |
| Patient Verification | Requesting the patient’s full name, date of birth, and sometimes a unique identifier to ensure HIPAA compliance. | Asking for full name, DOB, and MRN before sharing information. |
| Hold Protocols | Informing the caller before placing them on hold, including the reason and expected wait time. | “I’ll place you on a brief hold while I access your file—this will take about a minute.” |
| Clear Communication | Using plain language, avoiding jargon, and speaking slowly for understanding, especially with older patients or language barriers. | Simplifying explanations and repeating key details if needed. |
| Escalation Protocols | Steps to involve supervisors or clinical staff when an issue exceeds the staff member’s authority. | “I understand your concern, and I’ll connect you with our nurse supervisor.” |
| Service Recovery | Techniques for turning negative experiences into positive ones, often through empathy and prompt action. | “I’m sorry for the inconvenience. Let’s work together to find the earliest available appointment.” |
| Tone Modulation | Adjusting vocal tone to suit the situation and convey empathy, confidence, or authority as needed. | Softer voice for distressed patients, firm voice for escalations. |
| Information Filtering | Prioritizing the most relevant information and avoiding overwhelming the caller with excessive details. | Providing only key facts and offering additional details if requested. |
| Call Logging | Documenting every call’s details, including date, time, caller’s identity, and actions taken, to ensure compliance and continuity of care. | “5/29, 2:30 PM – Patient requested refill for hypertension meds. Verified DOB and MRN.” |
Real-Life Examples and Scripts
New Patient Call Scripts
Receptionist: “Good morning, thank you for calling [Practice Name]. My name is [Receptionist Name]. How may I assist you today?”
Caller: “I’d like to schedule a new patient appointment.”
Receptionist: “Absolutely, I’ll be happy to assist. May I have your full name, date of birth, and a contact number?”
Caller: “My name is [Name], date of birth [DOB], phone number [Number].”
Receptionist: “Thank you. Have you been referred by another physician or found us online?”
Caller: “I was referred by Dr. [Name].”
Receptionist: “Excellent. Let’s get you scheduled. Are mornings or afternoons more convenient for you?”
Caller: “Afternoons are best.”
Receptionist: “Perfect. I have an opening on [Date] at [Time]. I’ll send you an appointment confirmation via text and email. Do you have any questions or special needs we should note for your visit?”
Caller: “No, that’s all.”
Receptionist: “Great! We look forward to seeing you. Thank you for choosing [Practice Name].”
This script demonstrates clear communication, respect for patient preferences, and efficient information gathering.
Difficult Calls: Handling Complaints and Escalations
Receptionist: “Thank you for calling [Practice Name]. How may I assist you?”
Caller (angry): “I’ve been waiting for test results for two weeks! This is unacceptable.”
Receptionist: “I sincerely apologize for the delay and understand your frustration. Let me check the status of your results immediately. May I confirm your full name and date of birth?”
Caller: “[Provides info]”
Receptionist: “Thank you. I’ll review your file and speak with the appropriate department. May I place you on a brief hold while I investigate?”
Caller: “Fine.”
Receptionist: “Thank you. I appreciate your patience.” (After checking) “Your results are in, and the nurse will call you today with a detailed explanation. I will ensure this happens. Is there anything else I can assist you with?”
Caller: “No, that’s all.”
Receptionist: “Thank you again for your understanding. We value your care and will follow through promptly.”
This script shows how to acknowledge frustration, act decisively, and provide clear next steps.
Prescription and Lab Result Calls
Receptionist: “Good afternoon, this is [Name] from [Practice Name]. I’m calling to confirm your prescription refill request. May I verify your full name and date of birth?”
Caller: “[Provides info]”
Receptionist: “Thank you. Your prescription has been approved and sent to [Pharmacy Name]. You may pick it up today after 3 PM. If you have any questions or need further assistance, please let us know.”
This script is short, direct, and focused on compliance and clarity.
Common Mistakes and How to Avoid Them
Tone and Attitude Pitfalls
A major misstep in medical office calls is using an improper tone. Rushed or dismissive language can erode patient trust, while overly casual communication can undermine professionalism. For example, using slang, filler words, or failing to greet the caller respectfully diminishes credibility. Correct this by adopting a calm, courteous tone, pausing to let the caller finish speaking, and using professional greetings and closings.
Another common pitfall is impatience. Cutting off callers or rushing through information not only frustrates patients but can lead to errors. A simple fix: maintain a steady pace, use verbal nods like “I understand,” and clarify when necessary. Staff training should emphasize the importance of tone and empathy in every interaction, ensuring each call feels like a personalized experience.
Process Breakdowns
Process failures often stem from unclear internal protocols. For example, staff may forget to log call details, resulting in gaps in patient records. Another issue is poor handoffs—transferring calls without explaining the situation to the next person. This creates frustration and delays resolution. Standardize call procedures with clear documentation templates, checklists for call transfers, and role-specific training.
Additionally, failure to follow escalation protocols can prolong issues or cause compliance breaches. Establish clear guidelines for when and how to escalate calls, ensuring every team member knows who to contact for urgent matters. Continuous feedback and regular call audits help identify bottlenecks and reinforce best practices.
Legal Risks of Poor Etiquette
Medical offices face significant compliance risks when calls aren’t handled properly. Sharing sensitive information without verifying the caller’s identity breaches HIPAA, potentially resulting in fines or lawsuits. Even minor slip-ups—like mentioning a patient’s condition in front of others—can trigger legal consequences.
To mitigate these risks, train staff to always verify identity before sharing details. Use compliance scripts that cover verification, consent, and information delivery. Document every call, noting key details and actions taken. Regular refresher sessions on HIPAA and state-specific laws are essential to maintain vigilance and prevent costly mistakes.
Tools and Technologies for Managing Calls Efficiently
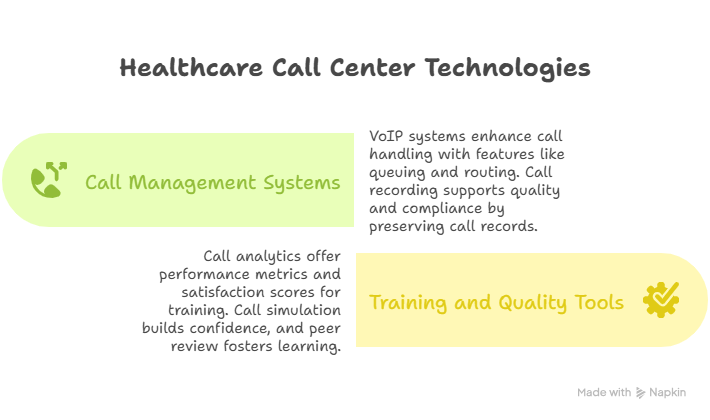
Call Management Systems
In busy medical offices, VoIP systems offer scalable, reliable solutions for handling high call volumes. Features like call queuing, auto-attendants, and call routing ensure patients are connected to the right staff efficiently. Call recording functions not only improve service quality but also support compliance by maintaining detailed records of interactions.
Call monitoring tools enable supervisors to track real-time performance, identifying bottlenecks and coaching opportunities. Implementing systems that integrate with patient management software streamlines call documentation and minimizes errors. For example, a call system that automatically logs patient interactions into the electronic health record (EHR) ensures continuity of care and reduces compliance risks.
Training and Quality Assurance Tools
Consistent quality in medical calls requires continuous training and real-time feedback mechanisms. Software tools like call analytics platforms provide data on average handling times, patient satisfaction scores, and call outcomes. These insights help identify training needs and reward high-performing staff.
Call simulation tools allow staff to practice scripts and handle complex scenarios without patient involvement, building confidence and competence. Peer review systems create a culture of accountability and continuous learning, ensuring best practices are consistently applied. Integrating call quality metrics into regular performance reviews reinforces the importance of professional, compliant communication.
How ACSMO’s Certified Scribes Are Trained to Represent Clinical Teams with Clarity—Even Over the Phone
Mastering medical office telephone etiquette is a vital skill for any professional pursuing the Medical Scribe Certification. In a healthcare setting, medical scribes not only document patient encounters but also handle phone calls involving sensitive information, appointment scheduling, and urgent clarifications. This certification equips scribes with the tools to execute these responsibilities with clarity, professionalism, and compliance.
The program covers essential topics such as HIPAA compliance, state-specific confidentiality laws, and patient communication protocols. Participants learn to manage calls efficiently, ensuring that every interaction supports accurate documentation and seamless patient care. From verifying identities to summarizing call details for the electronic health record (EHR), the certification prepares scribes to be reliable points of contact within the medical team.
Interactive modules focus on real-world scenarios where telephone interactions can affect patient outcomes and legal compliance. Through case studies, roleplays, and live simulations, learners gain the confidence and skillset to handle escalations, resolve patient concerns, and deliver clear, empathetic communication. Mastery of telephone etiquette not only enhances the scribe’s role but also strengthens the entire practice’s workflow and patient satisfaction.
For a deeper understanding of how this certification elevates phone-based interactions and supports career growth, explore our Medical Scribe Certification program today and take your skills to the next level.
Conclusion / Summing Up: Mastering Medical Office Phone Etiquette
In the fast-paced environment of medical offices, mastering telephone etiquette isn’t optional—it’s a professional imperative. Every call reflects the practice’s commitment to patient care, compliance, and operational excellence. By implementing clear communication protocols, maintaining legal compliance, and delivering empathetic interactions, staff can transform routine phone calls into opportunities for trust-building and patient satisfaction.
This guide has provided actionable insights into the core principles, terminology, and real-world scenarios that define excellent phone etiquette. From managing difficult calls to handling prescription inquiries, each skill is vital for ensuring accuracy, reducing legal risk, and elevating patient experiences.
For those seeking to excel in medical office communication, the Medical Scribe Certification offers comprehensive training that integrates these best practices into your daily role. By mastering these skills, you’re not only enhancing your career prospects but also contributing to a culture of professionalism and care within your organization.
Explore the Medical Scribe Certification program to start transforming your phone interactions today and set yourself apart in the healthcare field.
Frequently Asked Questions
-
The single most crucial aspect is professionalism combined with compliance. Every call represents the practice’s commitment to patient privacy, care quality, and operational excellence. This includes proper patient verification, clear communication, and adherence to HIPAA and state-specific laws. Even minor oversights—like sharing sensitive details without verifying identity—can have serious consequences. Medical Scribe Certification emphasizes the importance of mastering these skills, ensuring that scribes handle calls confidently and competently. In a healthcare setting, one misstep can erode trust, disrupt workflows, and create legal risks. Therefore, clear, compliant communication protocols are the foundation of safe and effective phone interactions.
-
Maintaining patient confidentiality is non-negotiable. A scribe should always verify the caller’s identity by asking for their full name, date of birth, and unique identifier before disclosing sensitive information. Conduct calls in private or controlled environments and use headsets to minimize the chance of others overhearing. Avoid discussing sensitive details within earshot of patients or staff who aren’t involved. Document each call clearly, noting the verification steps taken and any information shared. Mastery of HIPAA compliance, reinforced through the Medical Scribe Certification, ensures scribes consistently uphold patient privacy standards during every interaction.
-
Rushing calls, using improper tone, or neglecting to document are common pitfalls. Failing to verify identity before sharing sensitive information can breach HIPAA and create legal risk. Another frequent mistake is inadequate note-taking, leading to gaps in patient records. Additionally, mismanaging escalations—by failing to follow protocols or not notifying supervisors—can prolong resolutions or cause patient dissatisfaction. The Medical Scribe Certification program addresses these issues with roleplays, compliance-focused training, and call simulations, helping scribes develop habits that prevent errors and maintain professionalism. Effective call handling isn’t just about speaking clearly—it’s about following precise protocols with every interaction.
-
Proper telephone etiquette significantly enhances patient trust and satisfaction. A friendly, professional tone and clear, empathetic communication reassure patients, making them feel valued and respected. When staff listen attentively, answer questions thoroughly, and provide accurate information, patients are more likely to comply with instructions and return for future care. Conversely, rushed or impersonal calls can damage trust, leading to negative reviews and lost business. Medical Scribe Certification emphasizes the importance of building rapport through professional interactions, helping scribes contribute to a practice’s reputation for care excellence. Every call is an opportunity to foster loyalty and strengthen patient relationships.
-
VoIP systems, call routing software, and automated call logging tools streamline call management, ensuring efficiency and compliance. These systems can queue calls, direct them to the appropriate staff, and integrate with electronic health records (EHRs) for seamless documentation. Call monitoring and analytics platforms provide real-time feedback on performance, helping identify training needs and recognize high performers. Training tools, including call simulation software, prepare scribes to handle real-world scenarios confidently. The Medical Scribe Certification covers these technologies, demonstrating how they support both workflow optimization and patient satisfaction. Implementing these tools reduces bottlenecks and enhances overall call quality.
-
When faced with an escalation, active listening and empathy are key. Acknowledge the caller’s frustration and express genuine concern. Use a calm, steady tone to diffuse tension. Verify the caller’s identity, document the issue thoroughly, and follow escalation protocols—this may involve notifying a supervisor or connecting the caller with clinical staff. Never make promises you can’t keep; instead, provide realistic expectations and confirm follow-up actions. The Medical Scribe Certification equips scribes with scripts, protocols, and scenario-based training, ensuring they handle escalated calls with professionalism and poise, turning potential crises into opportunities for resolution.
-
Accurate documentation ensures continuity of care, legal protection, and quality control. Each call should be logged with the date, time, caller identity, reason for the call, and key actions taken. Without this record, vital information can be lost, compromising patient safety and exposing the practice to compliance risks. HIPAA mandates thorough record-keeping for any patient interaction, including calls. Medical Scribe Certification stresses the importance of precise documentation to safeguard against errors and support clinical decisions. Consistent, detailed call records enhance team communication, protect patient rights, and reinforce the practice’s commitment to professionalism and compliance.