Complete Breakdown: What's Included in the 2026-27 CMAA Exam
Every CMAA candidate has the same fear: you study hard, walk in confident, then the exam hits you with workflows you have never practiced under pressure. The 2026 to 2027 CMAA exam is not a trivia test. It is a systems test that rewards people who can run a clinic day smoothly, document cleanly, communicate clearly, and protect revenue and compliance at the same time. This breakdown shows what is actually included, what gets tested in scenarios, and how to prepare with precision using ACMSO resources, not random internet notes.
1. What the 2026 to 2027 CMAA Exam Is Really Testing
The CMAA exam is designed to measure job ready performance, not memorized definitions. If you have ever felt competent at work but panicked during testing, it is usually because you studied facts instead of workflows. The exam leans into real front desk pressure: time constraints, interruptions, incomplete information, and the need to choose the safest next step quickly.
Expect questions that mix patient experience, operational accuracy, and risk control. A single scenario may combine scheduling logic, basic billing awareness, and compliance decisions. That is why candidates who ignore process based study often fail even after finishing a course.
The fastest way to map what you are missing is to compare your skills against the workplace expectations in top employer skills, then layer your prep around demand trends and role evolution in the job market outlook and the shift toward virtual medical administration. If you do not understand how the role is changing, you will misread what the exam is trying to validate.
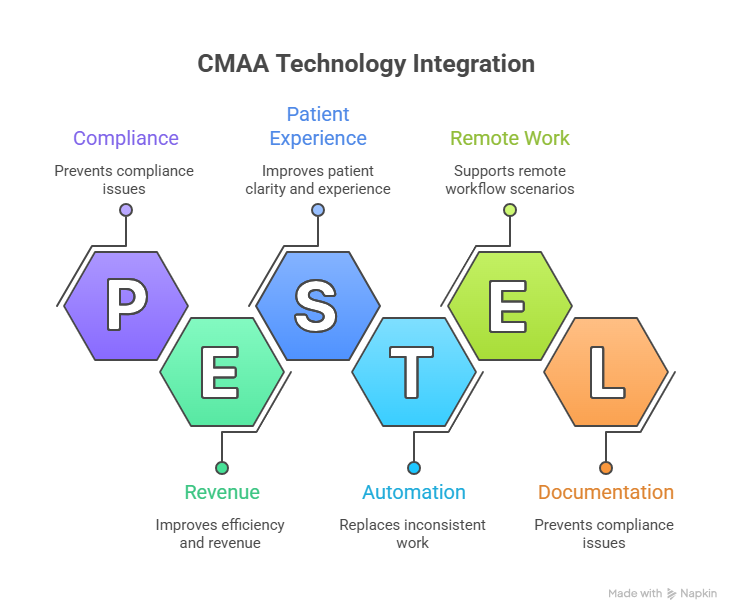
A big 2026 to 2027 pressure point is technology enabled productivity. Clinics are tightening margins, which means faster sign off, fewer documentation errors, fewer preventable denials, and cleaner audit readiness. If you want a high leverage framing for this, study tech driven outcomes like the operational mindset shown in the medical office automation trends and build your thinking around measurable outcomes.
You should also set expectations around career impact. Many candidates are doing this exam because they need a raise, a better shift, or a pathway into leadership. That reality is reflected in salary and opportunity content like the annual CMAA salary report, the interactive salary calculator, and the broader ROI argument in why CMAA certification boosts opportunities. The exam is hard because the credential is meant to signal dependable performance.
2. The CMAA Exam Content Areas You Must Master (and What They Look Like in Practice)
Most candidates waste time because they do not translate topics into actions. The exam rewards candidates who can identify the next correct operational move. If a question mentions an upset patient, your job is not to be “nice.” Your job is to protect trust, protect policy, and move the workflow forward without creating risk.
Start with the front office engine: registration accuracy, insurance capture, and scheduling discipline. These are the levers that prevent downstream chaos. If you want to see the “why” behind the role’s rising importance, read the evidence oriented content in how certified CMAAs improve efficiency and the broader trends summarized in the healthcare administration report.
Next, understand patient flow as a system. Scheduling is not just filling slots. It is controlling demand and protecting clinician time. This is where candidates get trapped by realistic pressure situations, like double booking, late arrivals, and incomplete paperwork. Pair your scheduling study with tool literacy from the scheduling software glossary and workflow language from patient flow management terms.
Billing awareness is another heavy test area, even if you are not a coder. The exam checks that you can explain common patient questions, identify what should be documented, and avoid statements that violate policy or scope. Build your foundation using medical billing explained clearly and add systems knowledge from medical billing software terms.
Communication is tested as a clinical safety tool, not a soft skill. You will face scenarios where the correct answer is about verification, tone, and escalation, not about having the most detailed explanation. Train this like a skill by using medical office telephone etiquette and practicing structured listening using active listening scenarios. For difficult interactions, sharpen your responses with the frameworks inside conflict resolution in medical admin.
Technology is no longer optional. In 2026 to 2027, the “excellent” CMAA is expected to support efficiency and documentation quality through consistent tool usage. That includes understanding EMR navigation terms in the EMR software glossary, operational tooling in patient management systems, and the automation direction covered in automation trends for CMAAs.
3. How the Exam Will Test You (Question Styles, Scenario Traps, and Time Pressure)
If you have ever said “I knew the material but the questions felt different,” you are describing scenario based testing. The exam often uses short stories with incomplete information because that is real clinic life. The correct answer is the one that reduces risk and preserves workflow integrity, not the one that sounds most helpful.
One trap is “premature problem solving.” A scenario might describe an insurance issue, but the first best step may be verifying coverage, documenting the check, and communicating the limitation clearly, not offering alternatives you are not authorized to guarantee. Build this mindset through content that links admin actions to outcomes, like the measurable framing in the interactive industry report on job demand and the career leverage explained in future proofing your CMAA career.
Another trap is “policy blind empathy.” Many candidates choose answers that feel kind but violate policy, privacy, or scope. The exam will test whether you can be compassionate while still verifying identity, protecting PHI, and escalating urgent issues correctly. Train your response style through the language frameworks in patient advocacy role play scenarios and the practical scripts in telephone etiquette.
Time pressure is its own skill. The goal is not speed. The goal is fast clarity. You want a repeatable decision pattern: identify the risk, identify the scope, choose the safest next action, document it, then escalate if required. If you want a model for how professionals train under test conditions, look at how ACMSO frames practice and readiness in the interactive practice exam and the preparation discipline in the exam day checklist. Even though those are scribe focused, the test skill is the same: calm decision making under constraints.
Finally, treat mistakes as signals, not shame. Many candidates keep repeating the same weak areas because they never isolate the root cause. If you miss questions, categorize them: process error, scope error, terminology confusion, or tool confusion. Then use targeted resources like medical terminology quick study and workflow glossaries like patient flow management to remove friction fast.
4. Technology and Documentation Topics Included (Because Clinics Now Grade You on Output)
If you treat technology as “nice to know,” you will feel surprised on exam day. Many 2026 to 2027 questions assume you understand why standardization matters: templates reduce rework, macros reduce errors, eligibility workflows prevent denials, and clean documentation prevents compliance issues.
Start with the vocabulary and navigation logic that shows up in EMR scenarios. If you do not know what common EMR terms mean, questions will feel like trick questions. Use the EMR software terms dictionary and connect it to the actual operational toolset described in patient management systems. The goal is not memorization, it is the ability to choose the correct workflow action inside a tool.
Next, build a mental model of automation. Automation does not replace you. It replaces inconsistent work. That means the CMAA who understands automation becomes more valuable, not less. This shift is covered directly in medical office automation trends and the role transformation lens in virtual medical administration. Expect questions that test your ability to work inside standardized processes, not “do it your own way.”
Documentation awareness is another technology tied area. You do not need to code, but you do need to understand what missing information does to revenue and patient experience. Candidates lose points because they cannot connect intake accuracy to downstream results. Study the evidence oriented framing in how certified CMAAs improve efficiency and bring that into your exam reasoning: if an action reduces rework, reduces denials, improves patient clarity, it is usually closer to the correct answer.
Also expect digital communication and remote workflow scenarios. Telehealth and remote admin coordination require clear instructions, identity verification, and documentation of outcomes. That is why foundational communication skills remain non negotiable. Pair your tech prep with communication tools like active listening scenarios and escalation framing via conflict resolution.
Finally, understand that technology is connected to career growth. Clinics promote the person who can make systems work, not the person who works harder in chaos. You can see the payoff in the career positioning and outcomes summarized in success stories from CMAAs and the market advantage outlined in why CMAA certification boosts opportunities.
5. A High Precision Prep Plan for 2026 to 2027 (So You Walk In Knowing You Covered Everything)
Most candidates fail because their prep is unstructured. They read random notes, watch random videos, and “feel busy.” Busy is not ready. You need measurable checkpoints, like a clinic would.
Week 1 is systems mapping. Identify every workflow that could appear: registration, scheduling, eligibility, phone interactions, documentation updates, and basic billing explanations. Use the skills benchmark in top employer skills as your audit list, then add the future leaning skills from future proofing your CMAA career. If you cannot describe a workflow in five steps, you do not own it.
Week 2 is terminology and tool fluency. Do not study vocabulary in isolation. Study it inside actions. Use EMR terms, the scheduling glossary, and the patient management systems guide. Then practice explaining the workflow in plain language, because that is how scenario questions are written.
Week 3 is scenario conditioning. This is where you build speed without panic. Train with structured questions like a simulation. A strong model for this is the practice focus inside the interactive practice exam and the mistake driven improvement style in top exam mistakes and how to avoid them. Again, the role is different, but the testing psychology is identical.
Week 4 is weak point elimination and exam day execution. Treat exam day like a performance: sleep plan, hydration, timing strategy, and a decision framework for tricky scenarios. Use the operational approach in the exam day checklist and combine it with the confidence building evidence of career outcomes in the annual CMAA salary report. When you connect prep to outcomes, you study differently.
After you pass, translate this into leverage. Salary negotiation is easier when you can articulate measurable value, like error reduction, faster patient flow, and cleaner documentation. Use the salary calculator and compare your market position against the job market outlook. The credential is not the finish line, it is the proof.
6. FAQs: CMAA Exam Breakdown for 2026 to 2027
-
If your study sessions produce knowledge but not faster decision making, you are studying the wrong way. The exam tests workflows and safe next steps, so your prep must be built around actions: intake accuracy, scheduling logic, billing awareness, communication, and tool usage. Use top employer skills as your checklist, then align it to the role’s evolution in the healthcare administration report. The fastest readiness signal is this: you can read a scenario and instantly name the risk, the scope boundary, the next action, and the documentation required.
-
Most wrong answers sound helpful but create risk. Candidates choose empathy without policy, speed without verification, or explanation without documentation. Scenario questions reward the safest next step, not the most detailed response. Train using structured communication resources like telephone etiquette and active listening scenarios, then add de escalation structure from conflict resolution. If you can consistently choose options that reduce risk and preserve workflow, your scores rise fast.
-
You do not need to be an IT person, but you must understand how technology supports standardized workflows. Expect questions tied to EMR navigation, correct chart handling, documentation updates, and how tools reduce errors and rework. Build tool fluency using the EMR terms dictionary and operational context from patient management systems. Then connect it to the bigger trend shift described in medical office automation trends. The exam rewards candidates who understand outcomes, not buttons.
-
Focus on preventing avoidable problems. You need to understand eligibility confirmation, patient responsibility language, and when to escalate issues like authorization risk. You also need to communicate clearly without giving advice outside your scope. Use medical billing explained clearly to lock the foundation, then expand your systems view using billing software terms. The exam often checks that you can choose actions that reduce denials and confusion, not that you can code a claim.
-
Treat scheduling as operational control, not calendar work. Every scheduling decision affects clinician time, patient satisfaction, and throughput. Learn the language and logic using the scheduling software glossary and train real workflow thinking through patient flow management terms. Then practice with short scenario drills: late arrival, wrong appointment type, missing paperwork, and urgent requests. When you can describe the safest next step in five seconds, you are ready for exam pacing.
-
Stop trying to “cover everything” and start eliminating score killers. Identify your top three weak categories using practice questions: workflow logic, scope and policy judgment, or tool and terminology confusion. Then use targeted ACMSO content to close gaps: future proof skill framing, EMR terms, and communication scripts like telephone etiquette. Keep a one page error log, rewrite the correct decision rule, and retest it daily.
-
Passing is the credential, but the real win is leverage. Clinics pay more for predictable performance: fewer errors, cleaner intake, smoother flow, better patient communication, and stronger documentation habits. Use the interactive salary calculator and benchmark against the annual CMAA salary report. Then translate your certification into measurable value using the outcomes mindset in how certified CMAAs improve efficiency and proof based confidence from real life success stories. That is how you move from “certified” to “promotable.”