CMAA Exam Prep: The Top 10 Mistakes You Need to Avoid
Most CMAA candidates do not fail because they did not “study hard.” They fail because they practiced the wrong way, ignored high risk workflow topics, and walked into the exam with weak decision patterns. The CMAA exam rewards safe next steps, clean communication, and operational accuracy that matches real clinics in 2026 to 2027. This guide breaks down the top 10 mistakes that quietly destroy scores and shows the exact fixes, drills, and proof habits that make first try passing predictable.
1. Mistake #1 to #3: Studying Like a Student Instead of Training Like a Clinic Operator
Mistake #1: Memorizing definitions without building decision rules
If you can recite a term but freeze when a scenario asks “best next step,” you are training trivia, not judgment. The exam is closer to real front office work covered in top CMAA skills employers want and the workflow pressure described in the medical admin job market outlook.
Fix: Build decision rules from mistakes. After every practice set, write one sentence rules like “When identity is unclear, verify before discussing anything.” Use phrasing frameworks from telephone etiquette examples and comprehension drills from active listening scenarios. Add escalation triggers from conflict resolution guidance.
Mistake #2: Skipping workflow topics because they feel “basic”
Many candidates avoid scheduling, intake, and documentation because it seems simple. Then the exam hits scenario chains where a small intake error becomes a billing problem, a scheduling problem, or a patient trust problem. These chains match real operational risk discussed in the 2026 healthcare administration report and the efficiency impact shown in research on certified CMAAs improving efficiency.
Fix: Treat workflow topics as score multipliers. Drill patient flow logic using patient flow management scenarios and match it to scheduling tool logic in the scheduling software glossary. Reinforce documentation habits with patient management systems examples.
Mistake #3: Practicing untimed and calling it “prep”
Untimed practice creates false confidence. The exam punishes slow reading, second guessing, and long mental debates. The job itself also punishes it, especially in modern settings described in virtual medical administration and the process standardization push covered in medical office automation trends.
Fix: Train pacing. Use micro sets and strict review. Do 15 to 25 questions timed, then spend longer reviewing than answering. Convert every miss into a rule and a script. Use communication patterns from telephone etiquette and calm under pressure habits reinforced by conflict resolution practice.
2. Mistake #4 to #6: Losing Points on Communication, Tech, and Billing Traps
Mistake #4: Treating communication as “common sense”
The exam grades communication like a safety skill. Candidates lose points when they skip identity verification, over explain, or respond emotionally. Strong communication is a measurable skill set mapped in telephone etiquette examples and sharpened through comprehension patterns in active listening scenarios.
Fix: Practice scripts, not vibes. Build three scripts: appointment changes, billing questions, and upset patient escalation. Add boundaries and calm control using conflict resolution training and patient support language from patient advocacy role play.
Mistake #5: Underestimating tech and documentation questions
Tech questions are usually workflow questions. The exam wants safe handling of patient information and consistent documentation steps that match modern operations discussed in medical office automation trends and the tool fluency foundation in the EMR software terms guide.
Fix: Build an EMR safety list. Write “never do” rules and “always document” minimums. Tie documentation to continuity using patient management systems examples. Connect tech habits to the remote future described in virtual medical administration.
Mistake #6: Panicking on billing and insurance basics
You are not expected to be a coder, but you are expected to communicate safely and avoid preventable workflow errors. Many candidates miss points by guessing on coverage questions or promising what they cannot guarantee. The safe baseline is in medical billing explained clearly plus system vocabulary in billing software terms and tutorials.
Fix: Practice five billing scripts that protect trust. Focus on clarity, next steps, and documentation. Tie this to the operational impact in efficiency research and the career leverage explained in why CMAA certification boosts opportunities.
3. Mistake #7 to #10: Overthinking, Poor Review, and Broken Final Week Strategy
Mistake #7: Not reading what the question is actually asking
A large chunk of errors come from answering a different question than the one asked. The exam often hides the key verb. If the question asks “best next step,” you must choose the safest first action, not the final resolution. This is the same real world discipline needed in fast paced environments described in the job market outlook and reinforced by workflow standardization trends in medical office automation.
Fix: Train question parsing. Every practice item, underline the verb in your head. Then rank answers by risk reduction, privacy safety, and scope alignment. Use verification phrasing from telephone etiquette and boundary discipline from conflict resolution.
Mistake #8: Reviewing wrong answers but not learning why the right answer wins
Many candidates “review” by reading explanations and moving on. That keeps mistakes alive. Your goal is not recognition. Your goal is ownership. Ownership comes from being able to explain why the correct option reduces risk and keeps workflow moving. That mindset matches the outcomes framing in the 2026 healthcare admin report and the performance logic in top CMAA skills employers want.
Fix: One sentence explanations only. Force yourself to explain the correct choice in one clean line. If you cannot, you do not own it. Then build a decision rule. Add supporting scripts using active listening scenarios and workflow references from patient flow management.
Mistake #9: Not training for the modern CMAA role
2026 to 2027 clinics expect CMAAs who can handle hybrid workflows, standardization, and tech enabled operations. Candidates who study old mental models get surprised by workflow and tooling questions. The role shift is clear in virtual medical administration, automation trends, and future skill planning in future proof your CMAA career.
Fix: Add a weekly “modern operations” session. Review EMR concepts using EMR terms and workflow tooling using scheduling software glossary. Link it to flow and handoffs using patient management systems.
Mistake #10: Cramming the last week instead of consolidating
The final week should reduce anxiety, not create it. Random cramming multiplies nerves and makes your recall unreliable. The candidates who pass on the first try do not learn more in the last week. They learn cleaner. They consolidate decision rules, scripts, and weak area fixes. The payoff path is real, shown in annual CMAA salary report and validated by the interactive salary calculator.
Fix: Build a 7 day sprint. Days 7 to 4 are mixed sets and strict review. Days 3 to 2 are weak area focus. Day 1 is calm routine and light review only. Keep motivation grounded using CMAA success stories and the opportunity framing in why CMAA certification boosts careers.
4. The Anti Mistake Study System: How to Prepare So These Traps Cannot Happen
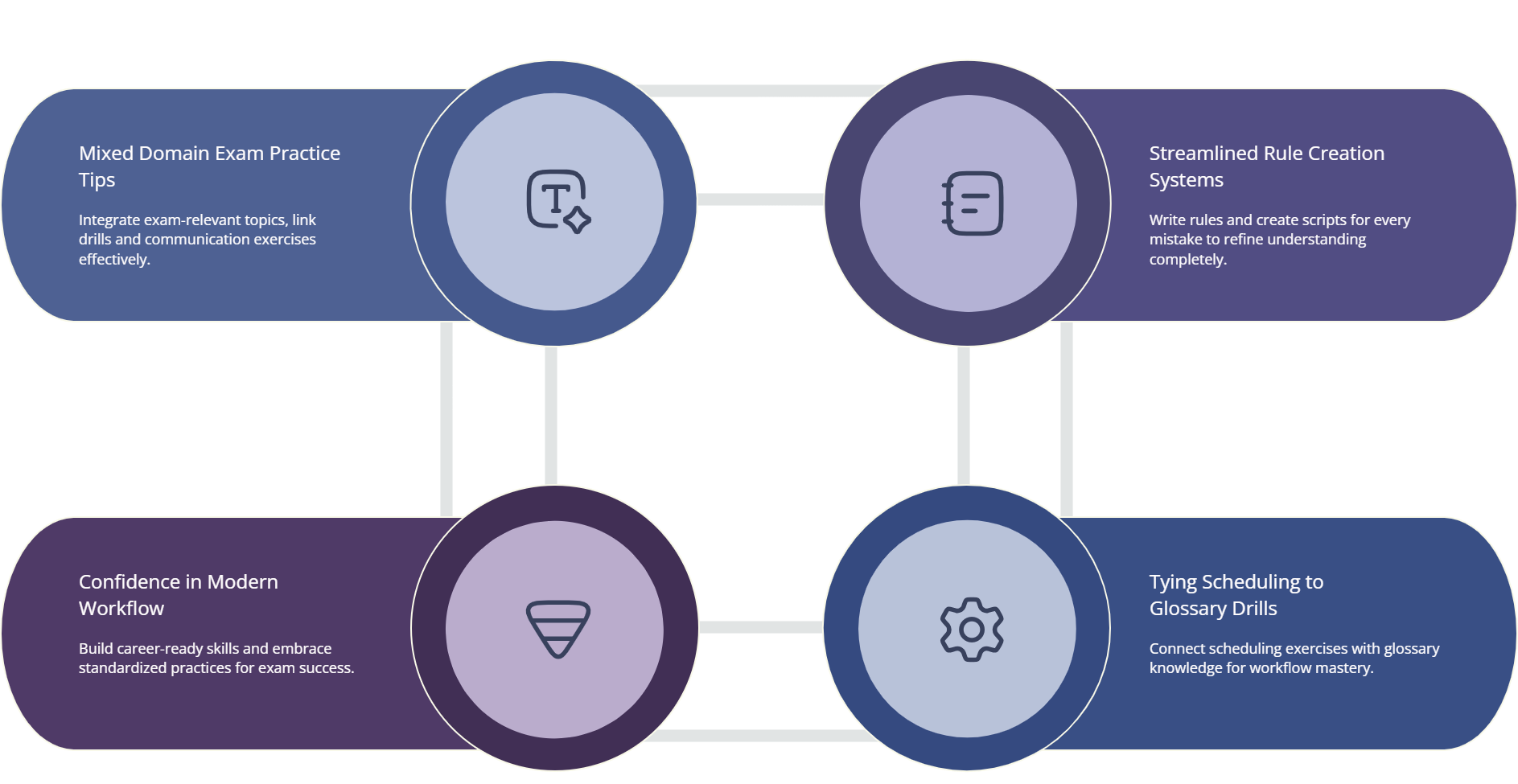
If you want to avoid these mistakes, you need a system that forces correction. Use a simple three layer approach.
Layer one: mixed domain practice. The exam blends scheduling, communication, billing basics, and tech workflow thinking. Your practice must blend them too. Tie scheduling drills to the scheduling glossary and flow reasoning to patient flow management. Pair each set with one communication drill using telephone etiquette and comprehension drills from active listening.
Layer two: rule writing and script building. Every missed question becomes a rule. Every rule gets a script. That is how you eliminate repeat errors. For billing items, base scripts on medical billing explained and reinforce vocabulary using billing software tutorials. For escalations, build boundary scripts using conflict resolution and patient support framing from patient advocacy.
Layer three: modern workflow confidence. The 2026 to 2027 environment expects process standardization, tech comfort, and strong handoffs. Build this layer using EMR terms, patient management systems, and the context in medical office automation trends. Tie it to the future career posture in future proof CMAA skills so your exam reasoning matches reality.
When this system is running, your confidence becomes evidence based. You can also keep motivation stable by anchoring your target to real outcomes in the annual CMAA salary report, validating your plan with the salary calculator, and reinforcing the payoff through success stories.
5. Exam Day Mistake Prevention: The Small Choices That Protect Your Score
Most exam day failures are preventable. They come from pacing errors, poor question parsing, and panic. Build a routine that protects execution.
Start with a simple pacing rule: do not sacrifice easy points for one hard question. If you get stuck, choose the safest next step and move forward. Your rules sheet should remind you how to pick safe options, especially on communication topics built from telephone etiquette and de-escalation patterns shaped by conflict resolution. Your brain performs better when it recognizes familiar scripts.
Next, control scenario questions by scanning for risk. Ask yourself what the test writer is really grading: privacy, scope, workflow continuity, or revenue safety. For billing and insurance, lean on safe explanations grounded in medical billing explained. For tech workflow questions, default to documentation discipline and chart safety aligned with EMR terms and clean handoffs supported by patient management systems.
Finally, remind yourself why this matters. Passing is not only a credential. It is leverage. The career upside is framed in why CMAA certification boosts opportunity and the market demand context is in the job outlook report. When your motivation is clear, your nerves shrink.
6. FAQs: CMAA Exam Prep Mistakes You Need to Avoid
-
Start an error log that forces conversion into rules. Every wrong answer becomes one decision rule and one short script. This works best when you use consistent language from telephone etiquette and comprehension framing from active listening scenarios. Tag each miss as scheduling, billing, tech, or communication. Then review your top two tags daily until they stop appearing.
-
They feel tricky when you do not anchor on the verb and the risk. Many options sound reasonable, but only one is the safest next action that protects privacy, scope, and workflow continuity. Train scenario logic using patient flow management and use escalation boundaries from conflict resolution. When you rank answers by risk reduction, the correct option becomes clearer.
-
You do not need advanced billing to score well. You need safe wording, clean next steps, and documentation awareness. Build your base using medical billing explained clearly and reinforce vocabulary using billing software terms. Then practice five scripts: coverage question, copay confusion, statement dispute, prior balance, and payment plan request.
-
Answering before verifying identity or overpromising outcomes. The exam wants you to verify first, state next steps, and document outcomes. Train your call openings using telephone etiquette examples and refine comprehension using active listening scenarios. For upset patients, use boundary language from conflict resolution guidance.
-
Stop studying it as calendar work. Study it as flow control. Drill triage decisions using the scheduling software glossary and connect each decision to throughput using patient flow management scenarios. Your goal is to explain why a scheduling choice prevents bottlenecks, not simply “fills the slot.”
-
Yes. Clinics are pushing standardization and tech-enabled workflows, which shows up in exam reasoning. Build safe habits using EMR terms and handoff clarity using patient management systems. Add modern context from medical office automation trends and virtual administration.
-
Consolidate, do not cram. Build a one-page rules sheet from your error log and run timed mixed sets daily. Focus review on why the correct answer is safest, not on reading explanations. Keep motivation anchored to outcomes using the annual CMAA salary report and the salary calculator. When your plan is structured, exam day becomes execution, not survival.