Interactive CMAA Practice Exam: Test Your Knowledge Before Exam Day
Most people fail the CMAA exam in a predictable way. They “study,” feel familiar with terms, then collapse under timed questions, workflow scenarios, and distractors that punish vague thinking. A real practice exam is not a confidence boost. It is a stress test that exposes weak recall, sloppy prioritization, and gaps in healthcare operations logic. This guide shows you how to use an interactive CMAA practice exam like a performance tool, not a quiz. You will build a score improvement system, fix the mistakes that kill pass rates, and walk into exam day with proof, not hope.
1) How to use an interactive CMAA practice exam the right way
A practice exam only works if it produces decisions. The goal is not a high score once. The goal is a repeatable score that holds under time pressure.
1) Start by mapping questions to job outcomes, not topics
CMAA questions often test whether you understand why a workflow exists. That is why exam prep improves real performance in scheduling, intake, documentation handoffs, and patient flow. Build that mindset by reading how admin performance improves system outcomes in the 2026 healthcare administration report and how admin teams become more efficient when systems are structured in the study on healthcare efficiency.
2) Use a two pass method for every practice exam
Pass one is speed and triage. Flag questions that require deep recall. Answer what you can confidently. Keep moving. This trains decision speed, which is what breaks people on exam day.
Pass two is precision. Return to flagged questions and write the reason the correct answer wins. If you cannot explain it, you do not own it yet.
This same discipline is what top performers use in role. Employers want CMAAs who can prioritize and execute under pressure, which is exactly what the top skills employers want breaks down.
3) Track three metrics that predict passing
Most candidates track only the score. That is weak. Track these instead.
Time per question: If you are slow, you are not failing knowledge. You are failing retrieval and prioritization.
Error category: Scheduling logic, compliance, communication, billing basics, EMR workflow. Categorize each wrong answer.
Second attempt accuracy: If you miss the same concept again, you are not fixing the root.
For salary and career impact, this level of preparation matters. It ties directly to the market reality in the CMAA salary report and the leverage you gain when you can prove readiness like the learners featured in real CMAA success stories.
4) Build a “mistake to drill” loop
Every wrong answer becomes a drill. Do not reread notes. Drill the exact weakness.
Wrong on scheduling priorities: drill scenario based scheduling from the scheduling software glossary.
Wrong on EMR terms: drill workflows from the EMR software terms dictionary.
Wrong on phone communication: drill scripts from telephone etiquette examples.
This is how you turn practice testing into real skill.
5) Use your practice exam score to predict job readiness
Hiring managers do not care that you “studied.” They care that you can perform. Practice exam performance can become a proof artifact, the same way scribes use proof to show competence in the medical scribe exam checklist. Build your own CMAA version.
Create a one page tracker with:
Baseline score
Weekly score trend
Top three error categories
Your fix plan for each category
This aligns with how certification creates opportunity in why CMAA certification boosts careers and how the job market is evolving in the CMAA job outlook.
2) Build a 7-Day CMAA “Score Jump” Sprint Before Exam Day
If you are close to exam day and your practice scores feel stuck, you need a short sprint that forces improvement fast. This sprint is built around one principle: every day must produce measurable score movement or it is wasted time.
Day 1: Baseline + error map
Take one timed set from your interactive practice exam. Do not pause. Record your score, time per question, and your top three error categories. Then rewrite every missed question into a single rule you can apply next time. This mirrors the job reality in the 2026 healthcare administration report because clinics reward repeatable decision quality, not “knowledge.”
Day 2: Workflow fixes only
Pick your worst workflow domain and drill it with real operational references. If your weakness is scheduling, drill decision rules using the scheduling software glossary. If your weakness is patient movement, drill bottlenecks using patient flow management scenarios. The goal is not reading. The goal is building a mental sequence you can execute in seconds.
Day 3: Communication and compliance traps
Most candidates lose points on “reasonable sounding” answers that violate boundaries or skip verification. Drill scripts and scenarios using telephone etiquette examples and active listening scenarios. Your objective is to recognize the safe answer immediately without overthinking.
Day 4: EMR and systems logic
If you are slow on EMR style questions, you are not missing facts. You are missing flow. Train by mapping a chart journey from check in to task closure using the EMR terms walkthrough and reinforce clean routing concepts with patient management systems examples. Then do a timed set focused on these question types.
Day 5: Billing and admin operations clarity
Even basic billing questions punish mixed up process stages. Drill claim lifecycle logic using medical billing explained clearly. Then write a six step claim flow in your own words. This creates fast recall and reduces confusion under time.
Day 6: Timed mixed mini mock + ruthless review
Run a timed mixed set. Mark every question you were unsure about, even if you got it right. Review only marked questions and wrong answers. Update your rules list. Your goal is to reduce hesitation, not just wrong answers. This aligns with the employer skill expectations outlined in top CMAA skills.
Day 7: Exam day simulation and confidence locking
Run one final timed set at the same time of day as your real exam. Use the same breaks and same rules. If you can hold your score under real conditions, you are ready. If you cannot, you now know exactly where to focus in the final hours. This is how you turn preparation into career leverage, which ties directly to the opportunity shift explained in why CMAA certification boosts careers.
3) High impact CMAA domains that practice exams expose fast
An interactive practice exam is valuable because it reveals which domain breaks you under time. Most candidates discover they are not weak in “knowledge.” They are weak in workflow logic and judgment.
Scheduling and patient flow is the silent score killer
Scheduling questions look simple until they demand prioritization with constraints. The wrong answer often sounds polite and reasonable. The right answer protects the day.
Train this by drilling scheduling logic using the scheduling software guide and patient movement decision points in patient flow management scenarios. These resources mirror how clinics actually run, which is why they translate into exam performance.
If you want job aligned motivation, connect this to where the market is going. Clinics are hiring for efficiency, and the trend is spelled out clearly in the medical office automation report and the broader signals in virtual medical administration.
EMR workflow questions punish guessing
EMR questions are rarely about brand names. They test whether you understand charts, tasks, routing, and data integrity. Candidates lose points because they do not understand why each step exists.
Build your foundation with the EMR terms walkthrough and reinforce admin facing systems language with patient management systems examples. When you can visualize the flow, you stop guessing.
Communication, de-escalation, and boundaries show up as scenario traps
The CMAA exam rewards candidates who can stay calm, keep patients informed, and protect boundaries without sounding cold.
That skill is trainable. Drill scripts and scenarios from active listening scenarios, boundary language from conflict resolution dictionary, and patient centered phrasing from patient advocacy role play.
This is also why certification changes outcomes. It strengthens how you operate under pressure, which is exactly what employers care about in top CMAA skills.
4) Score improvement system: from baseline to exam day confidence
If you want professional results, you need a professional system. Here is a score system that works because it attacks the reasons people fail.
Step 1: Establish a baseline and remove excuses
Take the interactive practice exam under realistic timing. No pauses. No notes. No second screen. You are testing your current operating system.
Then record:
Score
Time per question
Top three error categories
If this feels uncomfortable, good. Comfort is not the goal. Passing is.
Step 2: Convert mistakes into “next actions”
Every wrong answer should create one of these next actions.
Vocabulary gap: build a mini glossary and drill usage
Workflow gap: map the process step by step
Judgment gap: write a rule that would make you choose correctly next time
Support your workflow gaps with ACMSO’s interactive learning assets. Use medical billing explained to tighten claim flow logic and reinforce systems thinking with inventory management examples.
Step 3: Use spaced repetition for weak domains only
Most people waste time reviewing what they already know. That is why their scores stall.
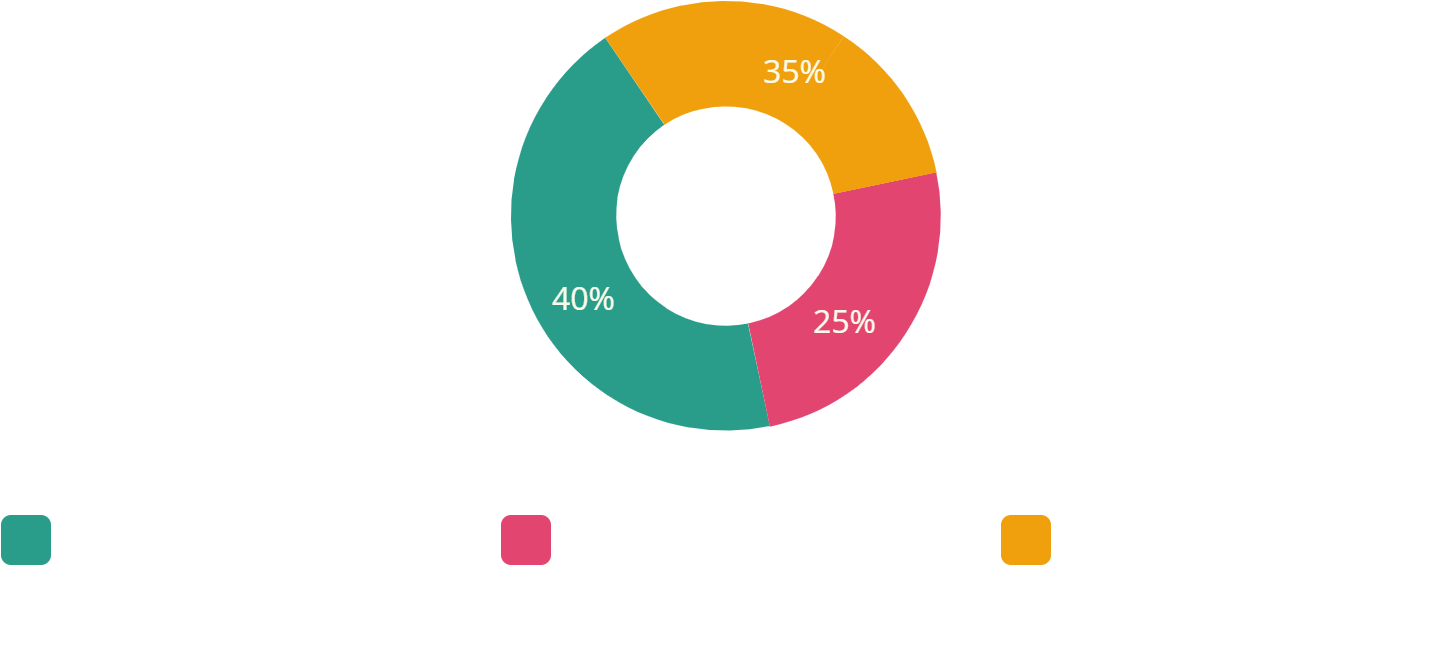
Instead, follow a rule.
70 percent of study time goes to your bottom two domains
20 percent goes to mixed practice
10 percent goes to speed drills
This approach matches what market ready professionals do. It builds competence in the exact areas that drive results, similar to how CMAAs build future readiness in emerging skills for the next decade.
Step 4: Add a weekly “timed mini mock”
Once a week, run a shorter timed set. The goal is to train decision speed and reduce second guessing.
This is also the easiest way to build a proof artifact you can use later. Your score trend becomes evidence. Evidence supports career mobility, which is why certifications connect to salary direction in the salary calculator page and the broader pay patterns in the annual CMAA salary report.
5) Exam day execution: turn practice into points
Most candidates lose points because they do not have a strategy for exam day. They have knowledge. They lack execution.
Rule 1: Use confidence tiers
As you answer, put questions into three mental tiers.
Tier A: You know it. Answer and move.
Tier B: You can eliminate options. Mark and move.
Tier C: You are guessing. Mark and move fast.
This protects time and prevents panic. It is the same discipline professionals use in high pressure roles, which you see in performance driven content like medical administration job trends and the expectation shift toward efficiency in the technology and automation trends.
Rule 2: Stop changing answers without a reason
People talk themselves out of correct answers because anxiety looks like logic. Only change an answer if you can state one clear rule that proves the new answer is correct.
Rule 3: Use micro resets
When you feel your focus slipping, reset quickly.
Sit back
Exhale slowly
Read the question again as a workflow decision, not a trivia prompt
This prevents cascades.
Rule 4: Bring the job into the exam
If a question asks what to do, imagine you are in the clinic and someone is watching your choice. The correct answer is usually the one that prevents downstream chaos.
This is why CMAA certification increases career opportunity. It trains judgment, not just facts, which is exactly what the career opportunity article highlights and what graduates echo in CMAA success stories.
6) FAQs
-
Take enough to create a stable score trend, not a lucky score. A strong standard is one baseline exam, then one timed mini mock each week, plus targeted question sets for weak domains. If your score improves but timing stays poor, prioritize timed drills. If timing improves but accuracy does not, your issue is concept clarity. Tie your weakest domains to interactive learning assets like the EMR terms walkthrough and scheduling software guide so your study time produces measurable correction.
-
Do not review everything. Review only what changes your next score. Categorize every wrong answer into vocabulary, workflow, or judgment. Then write one rule that would make you choose correctly next time. Build a drill from that rule and repeat it within 48 hours. This is how you create retention under pressure. If your mistakes are communication based, drill scenarios using active listening scenarios and conflict resolution practice to turn soft skills into repeatable decisions.
-
Scenario questions punish vague thinking. They force you to choose the option that protects workflow, privacy, and patient experience at the same time. The fix is to build decision rules. For example, verify eligibility before scheduling certain services. Escalate when a boundary is crossed. Summarize next steps at the end of every call. Use real workflow references like patient flow management scenarios and telephone etiquette examples to train your brain to pick the operationally safe answer.
-
You improve timing by improving retrieval speed. That comes from repetition under constraints, not rereading notes. Use timed sets where you must choose quickly, then review errors deeply. Keep a list of “slow concepts” and drill them daily for 10 minutes. If timing is slow due to workflow confusion, build flow maps using the patient management systems guide and the medical billing reference so your brain recognizes patterns faster.
-
The topics that pay off most are the ones that reduce errors and increase throughput. Scheduling logic, patient flow management, accurate documentation routing, and confident patient communication create daily impact. Those strengths translate into trust, better responsibilities, and higher earning potential over time, which connects to the leverage discussed in the annual CMAA salary report and the demand patterns in the CMAA job outlook.
-
Employers believe proof. Keep your score trendline, your error category tracker, and your drill artifacts. Then convert them into resume language that describes outcomes such as fewer scheduling errors, cleaner intake verification, and stronger patient communication. Pair your certification with skills employers already screen for using the top CMAA skills guide and support your story with market context from why certification boosts opportunities. This makes you sound employable immediately, not “new.”