Medical Scribe Career Outlook 2026-27: Salaries, Growth, and Trends
Medical Scribe careers are moving into a “proof-based” era in 2026–27: facilities don’t just want faster notes—they want measurable reductions in denials, cleaner charts, and happier clinicians. That’s good news if you build the right skill stack and can show evidence of impact. In this outlook, you’ll learn what’s driving demand, how salaries actually get set, which trends are real vs hype, and how to position yourself for the best roles—especially as AI documentation expands. (If you want a quick macro view first, start with the medical scribe market trends and the annual employment report.)
1) What’s driving medical scribe demand in 2026–27
The most consistent growth driver isn’t “more patients” (that’s always true). It’s documentation complexity plus throughput pressure colliding with clinician bandwidth. In 2026–27, the winners are health systems that can document accurately, close encounters quickly, and survive payer scrutiny without burning out providers. That’s why scribes keep showing up in workforce strategy, especially when leadership sees revenue leakage and compliance exposure tied to chart quality. If you want the cleanest framing, connect the demand story to revenue and risk: scribes help tighten documentation, reduce rework, and stabilize operations—exactly the “business case” lens in the hospital revenue impact analysis and the quality lens in the documentation accuracy report.
The 2026–27 demand engines that matter
1) Burnout isn’t a HR issue anymore—it’s an operational KPI.
Executive teams increasingly treat burnout like a throughput and retention metric. Scribes become the “bandwidth multiplier” when staffing is tight and visit volume stays high. If you need language for how to prove it at a facility level, the burnout reduction interactive report is the best anchor for translating feelings into measurable signals.
2) Payers and auditors are forcing “defensible documentation.”
Facilities are pressured to show clean problem lists, medically necessary notes, and consistent documentation across providers. Scribes who can standardize narrative flow while staying within scope become valuable—especially when a department is being watched for denials or coding queries. Pair this with the certification preference angle in why facilities prefer certified scribes because “certified” often signals lower onboarding risk.
3) Ambient AI is not replacing the role—it’s changing the job description.
Facilities adopting AI documentation still need humans to (a) correct errors, (b) enforce formatting and clinical clarity, (c) manage templates/macros, (d) ensure compliant note structure, and (e) keep clinicians from babysitting software. That’s the core argument in how scribes fit into an AI-driven world and the market landscape in the AI scribe & ambient dictation buyers guide.
4) Remote workflows are scaling—when quality is controlled.
Remote scribes aren’t just “work-from-home jobs.” They’re structured production systems with training, QA, secure tooling, and performance metrics. If you want to see where remote is mature, scan the remote market growth report and the top remote employers list. If you can demonstrate low edit rates, fast closure, and high accuracy, remote becomes a salary lever.
5) “Where the jobs are” is shifting by specialty and care setting.
The broad headline “scribes are growing” hides the real story: demand concentrates where documentation burden and throughput pressure are worst. To track that, use the employment trends visualization and the hiring density view in the top cities hiring report.
2) Salaries in 2026–27: what drives pay—and how to negotiate like a pro
Most people ask, “What’s the salary?” The higher-value question is: What variables move my pay band up fastest, and how do I prove I deserve it? Salary in 2026–27 is increasingly tied to risk reduction + measurable productivity, not just typing speed. Employers pay more when you reliably reduce provider edits, improve closure times, and protect documentation quality. That’s why pairing your job search with a proof strategy—like the evidence framework in the burnout report and the rigor angle in certified scribe preference—matters more than memorizing a national average.
Salary is set by 6 levers (and you can control most of them)
Lever 1: Setting (hospital system vs private clinic vs vendor vs telehealth).
Large systems often pay within structured bands but may offer stability, benefits, and upward mobility—especially if they’re actively hiring (see the top hospitals hiring directory). Vendors can scale hours and provide remote paths (start with the top remote employers list). Telehealth can open national roles if you match workflow demands (see the telehealth companies using scribes directory).
Lever 2: Specialty complexity (the quiet pay accelerator).
Higher complexity specialties (and high documentation burden workflows) tend to reward scribes who reduce errors and omissions. Your goal isn’t “know everything”—it’s learn one specialty deeply and become the person whose notes don’t trigger endless clarifications. This lines up with the “accuracy premium” theme in the documentation accuracy analysis.
Lever 3: Remote readiness (security + QA discipline).
Remote roles pay better when you’re low-risk: consistent structure, privacy discipline, predictable metrics, and strong QA. Remote isn’t casual—workflows are audited. Use the remote market growth report to understand why employers standardize and measure everything.
Lever 4: Certification and measurable competency.
In a crowded applicant pool, certification can be a filter—not because it magically makes you better, but because it reduces employer uncertainty. If you’re serious about positioning, align your preparation using the scribe certification exam guide, drill with the interactive practice exam, and avoid predictable failures with the top exam mistakes guide.
Lever 5: Proof artifacts (this is where negotiation is won).
Negotiation gets easier when you walk in with evidence: a one-page snapshot of closure rate improvement, reduced provider edits, or QA scores. The “proof artifact” approach isn’t theoretical; it’s the same logic used in the interactive workforce report and the metrics language in the employment trends visualization.
Lever 6: Your ability to operate inside modern EHR workflows.
Facilities pay for people who don’t slow clinicians down. That means mastering templates, smartphrases, and clean structure inside the EMR—not improvising every visit. If you want supportive skill-building for system fluency, the EMR software terms dictionary is a fast way to sound competent in interviews.
How to negotiate without sounding “greedy”
Negotiation in healthcare ops works when you tie your ask to cost and risk:
Lead with outcomes: “I reduce provider edits and improve same-day closure. Here’s how I track it.” (Anchor your talk track using the burnout reduction report and the revenue impact analysis.)
Use market anchors—then localize: National numbers are a starting point; your real leverage is your city/specialty/setting. Compare offers using the salary comparison tool and validate demand via the top cities hiring report.
Offer a performance plan: “If I hit X closure and Y QA score in 60–90 days, we revisit compensation.” It signals confidence and lowers employer fear. This fits the metrics-first trend described in the workforce report.
3) Growth paths in 2026–27: where the best opportunities actually are
A lot of scribes get stuck because they treat the role as “a job,” not a platform. In 2026–27, the strongest growth paths are built on a simple truth: facilities promote the people who make documentation reliable at scale. That can lead to lead-scribe roles, QA, training, template governance, specialty ownership, and remote team leadership—especially in organizations tracking outcomes. Use the macro signals in the medical scribe job growth analysis and the demand maps in the top cities hiring report to choose where you invest your time.
The 4 most common ladders (and how to climb them faster)
Path A: Specialty scribe → “trusted partner” scribe (higher stability, higher leverage).
The fastest way to become valuable is to reduce cognitive load for one specialty team. You do that by learning a specialty’s note expectations, common orders, and documentation pitfalls—and then building consistent structure. If you need an argument for why facilities pay more for accuracy, tie it to the documentation accuracy improvements and to decreased downstream rework.
Path B: Remote scribe → QA-ready scribe → remote team lead.
Remote programs need disciplined performers who can maintain quality without in-person supervision. If you want to target remote, read the remote market growth report and then focus on building proof: low edit rates, fast closure, and high QA. Once you have that, use the top remote employers list to aim for programs with established QA and advancement.
Path C: Scribe → workflow optimizer (templates/macros) → operations support.
Facilities are optimizing EHR workflows aggressively. Scribes who can standardize templates and reduce clinician clicks become valuable beyond “note-taking.” Build your language with the EMR terms walkthroughs and connect your impact to throughput with the hospital revenue analysis.
Path D: Scribe → medical admin hybrid (scheduling/inbox support) → broader healthcare ops.
Some of the fastest-growing roles blend documentation support with admin flow support. If you want to expand safely, sharpen adjacent skills like scheduling and patient flow—start with medical scheduling terms and patient flow management terms. This path can make you more employable in clinics that want “one person who keeps the day moving.”
4) The AI factor in 2026–27: how scribes stay essential (and get paid more)
The smartest way to think about AI documentation is: it moves the bottleneck. Instead of “typing the note,” the bottleneck becomes “ensuring the note is correct, complete, defensible, and consistent—fast.” AI can generate text; it can’t reliably judge clinical nuance, ensure scope-appropriate content, or protect against generic, risky phrasing without human oversight. That’s why the role evolves into editor + workflow controller + quality enforcer, as explained in scribes in an AI-driven world and reflected in how facilities evaluate tool stacks in the AI ambient dictation buyers guide.
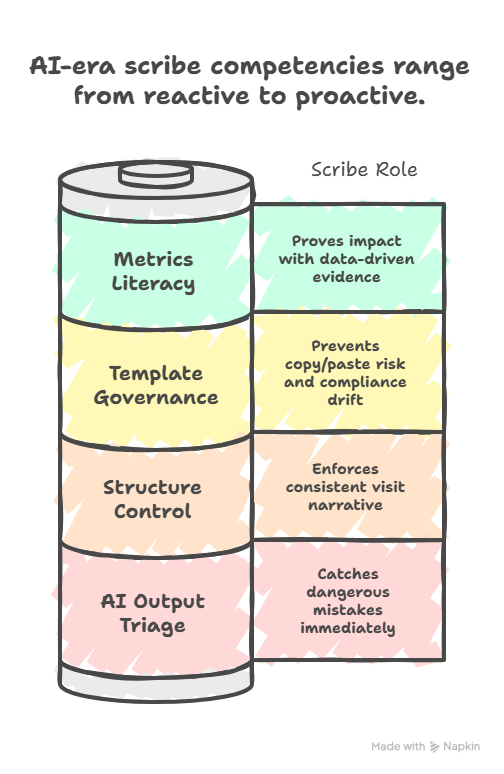
The 5 “AI-era” competencies that separate top scribes
1) AI output triage (catching the dangerous mistakes).
AI can misattribute symptoms, swap laterality, omit negatives, or overstate certainty. Your job becomes rapid triage: what must be corrected now vs what can be clarified later. This is why accuracy remains a headline capability in the documentation accuracy analysis.
2) Structure control (making notes scannable and coder-friendly).
Even when text is “correct,” it can be poorly structured. The best scribes enforce a consistent visit narrative, preventing chaos across providers. Facilities prefer this predictability—one reason behind preference for certified scribes.
3) Template governance (preventing copy/paste risk and compliance drift).
AI makes it easy to “sound good” while being dangerously generic. If your notes are filled with non-specific filler, they can raise audit red flags. Scribes who can maintain patient-specific documentation become more valuable, not less.
4) Metrics literacy (you can prove impact, not just claim it).
In 2026–27, facilities increasingly reward whoever can show the numbers: closure time improvement, decreased provider edits, improved QA, reduced query rates. This is the same measurement style used throughout the burnout reduction report and the systems thinking in the workforce report.
5) Tool fluency (you can operate in the EHR without slowing the room).
AI doesn’t remove the need to navigate the EMR quickly and correctly. If you want a practical foundation, the EMR glossary + walkthroughs helps you speak the language facilities expect.
5) Growth and hiring trends for 2026–27: how to spot the best jobs early
“Growth” is not a single number; it’s a pattern of signals. In 2026–27, the best opportunities show up where (a) hiring is concentrated, (b) documentation burden is highest, (c) QA systems exist, and (d) there’s a clear ladder. Instead of guessing, use data-backed internal resources to triangulate your search: start with the nationwide job growth analysis, then cross-check with the top cities hiring report, and finally filter by employer type (hospitals, telehealth, remote programs).
Where growth concentrates (and why it matters to you)
High-volume systems + specialty clinics tend to hire when documentation time is choking throughput. If you want direct targets, scan the top hospitals hiring list and compare it against your preferred regions using the employment trends visualization. For remote-first growth, use the remote employers directory plus the market context in the remote growth report.
How to evaluate a job posting like an insider
A strong 2026–27 scribe role usually includes some of the following:
Clear metrics: closure time, QA score, edit rate, productivity. If the posting talks about measurement, it usually means the organization understands the role’s value (mirror the metric logic in the burnout reduction report).
Training + QA infrastructure: not just “shadow for a week.” Programs that invest in training create longer-term roles and promotions (see patterns in the workforce report).
A defined ladder: lead scribe, QA, trainer, specialty lead, template owner.
Tool expectations are realistic: if they require AI tools, they should also define the human review role (use the framing in AI-driven documentation and the landscape view in the AI tools guide).
The “proof portfolio” that gets you better offers
If you want better salary and better roles, build a simple portfolio that demonstrates your impact:
Before/after note samples (de-identified) showing structure, completeness, and clarity.
A personal KPI dashboard: closure rate, edit rate, QA score, query rate.
A short workflow memo: one page on how you reduce rework and protect compliance.
Certification and practice results if you’re early-career: use the study techniques guide, strengthen terminology using the medical terminology quick study guide, and validate readiness with the interactive practice exam.
When you show proof, you stop being “a scribe applicant” and start being “a documentation outcomes hire.” That shift is exactly why facilities rationalize higher pay and prefer lower-risk candidates (again, see why certified scribes are preferred).
6) FAQs: Medical Scribe Career Outlook 2026–27
-
Quality will matter more—because quality protects revenue and reduces operational drag. Facilities increasingly measure downstream impact: provider edits, coder queries, audit findings, and encounter closure times. Fast but sloppy notes create rework, which defeats the point. If you want a facility-friendly way to talk about this, lean on the measurement approach in the burnout reduction interactive report and the accuracy emphasis in how scribes improve accuracy.
-
Remote roles are likely to continue expanding where organizations can maintain QA and security. The key is not “remote is popular,” it’s “remote is scalable when controlled.” If you’re targeting remote, read the remote market growth report, then target mature employers via the top remote employers list. Your advantage comes from proving you can hit metrics without supervision.
-
AI will change tasks, not eliminate the need for humans in many workflows. The “scribe value” shifts toward ensuring correctness, completeness, defensibility, and consistency—especially when AI-generated text risks being generic or inaccurate. To understand the practical role shift, use how scribes fit into an AI-driven world and compare tools and workflows through the AI scribe tool guide.
-
Don’t anchor on one “average.” Salary varies by city demand, specialty complexity, employer type, remote status, and your proof of performance. Use the salary comparison tool by state and specialty to set a baseline, then validate demand via the top cities hiring report and the macro trend view in the job growth analysis. Finally, negotiate using proof artifacts (QA scores, edit rate improvements, closure metrics).
-
Certification is increasingly valuable as a screening filter and trust signal—especially when facilities are worried about onboarding speed, accuracy, and compliance. If you’re aiming for better roles or remote programs, certification helps you stand out faster. Prepare strategically using the complete certification exam guide, avoid common failures with the exam mistakes guide, and confirm readiness with the interactive practice exam.
-
Build an “outcomes portfolio.” Track 2–3 KPIs (closure rate, provider edit rate, QA score), collect proof artifacts (exports, audits, scorecards), and add one specialization or remote-ready skill set. Then align your story with what facilities care about: burnout reduction, documentation accuracy, and revenue protection. The most direct internal foundation for that positioning is the combo of the burnout outcomes report, the accuracy analysis, and the revenue impact study.