Medical Scheduling 101: Key Terms & Practical Examples
Navigating medical scheduling is critical for seamless patient care and operational efficiency. At its core, this discipline ensures that healthcare providers maximize appointment availability, minimize no-shows, and maintain accurate records. Yet, medical scheduling is more than just booking slots—it demands a precise understanding of workflows, compliance standards, and patient needs. The rising demand for telehealth appointments and hybrid care has added layers of complexity, requiring modern solutions and skilled schedulers.
Healthcare facilities are increasingly leveraging advanced scheduling systems that automate confirmations, handle last-minute changes, and integrate with electronic health records (EHRs). These tools not only streamline front-desk tasks but also reduce human error. A strong grasp of key scheduling terminology, combined with hands-on practice, positions healthcare teams to improve patient satisfaction and revenue.
Throughout this guide, we’ll dissect core scheduling concepts, explore industry-proven practices, and deliver actionable insights. Whether you’re a medical office manager, front-desk coordinator, or aspiring healthcare scheduler, mastering this field ensures smoother patient flows and stronger provider relationships. Ready to elevate your knowledge? Let’s dive in.
Understanding Medical Scheduling
Definition and Core Concepts
Medical scheduling refers to the structured process of organizing patient appointments with healthcare providers. It’s not a simple task of filling a calendar but a complex orchestration balancing patient needs, provider availability, and compliance with privacy regulations. Schedulers must account for appointment types (e.g., routine check-ups, urgent visits), ensure accurate patient information entry, and adhere to standard procedures for appointment confirmations and cancellations.
A critical aspect of medical scheduling is recognizing scheduling hierarchy—understanding which patients need priority access and how different appointment lengths impact the day’s workflow. For instance, complex visits or procedures may block longer time slots, while follow-ups or minor consultations can be shorter, increasing patient throughput. Modern systems often automatically flag duplicate or overlapping appointments, reducing errors and optimizing schedules.
Schedulers must also master HIPAA-compliant processes, protecting sensitive health data while facilitating timely communications with patients. Integration with EHRs is now standard, enabling seamless updates and real-time access to patient histories and appointment statuses.
Efficient scheduling ultimately reduces wait times, increases provider productivity, and enhances patient satisfaction. Without it, clinics face bottlenecks, frustrated patients, and revenue loss.
Common Scheduling Formats
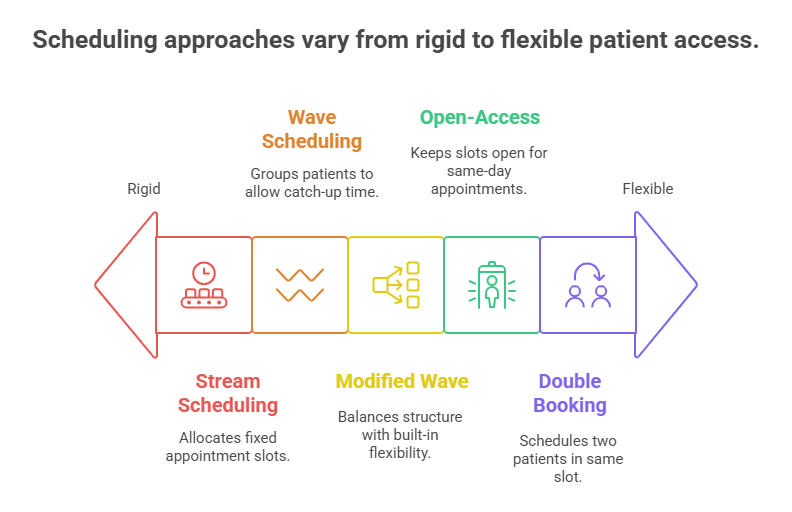
Healthcare facilities employ various scheduling formats tailored to their patient volumes, provider structures, and service types. The stream scheduling model assigns fixed intervals to each appointment, suitable for clinics with consistent patient flows. This method reduces overbooking but may underutilize provider time if appointments finish early.
Wave scheduling groups patients into blocks (e.g., three every half-hour), allowing providers to catch up if a patient is late or a visit takes less time. It increases flexibility but requires careful management to avoid congestion.
Another format, modified wave scheduling, combines fixed intervals with waves, offering a balance between structure and adaptability. It’s especially useful in multi-provider practices, where one practitioner’s delay can impact others.
Open-access scheduling, also known as same-day scheduling, reserves slots for urgent or walk-in patients, enhancing accessibility but demanding real-time coordination and rapid documentation. Double booking, though often a last resort, is sometimes used when patient demand exceeds capacity, but it risks delays and patient dissatisfaction if not managed carefully.
Choosing the right format depends on patient volume, visit complexity, and provider preferences. Mastery of these formats allows clinics to maintain control even during high-demand periods, ensuring optimal patient flow and minimizing revenue loss.
Key Terms and Their Practical Application
Essential Scheduling Terminology
Mastering medical scheduling requires a solid grasp of critical terminology. Terms like time-blocking refer to reserving specific periods for appointments, ensuring efficient workflows. Patient recall systems automate follow-up scheduling for preventive care or chronic condition management. These systems integrate with EHRs, ensuring timely reminders and reducing missed appointments.
Preauthorization requirements are essential in insurance-heavy environments. Schedulers must confirm approval from payers for procedures or specialist visits, avoiding costly denials. Encounter types, such as new patient, established patient, or procedure visit, dictate scheduling complexity and time allotment. Each type aligns with specific billing codes, requiring precision to avoid errors.
No-show rates measure how often patients miss appointments. High rates signal scheduling inefficiencies, calling for proactive strategies like reminders or waitlist management. Waitlists allow schedulers to fill gaps from cancellations, optimizing provider utilization. Double booking is a riskier tactic but may accommodate urgent needs during provider shortages.
Triage scheduling assigns appointments based on medical urgency, ensuring critical patients are prioritized. This requires collaboration with clinical staff to assess patient needs swiftly. Capacity planning uses historical data to predict appointment demand, helping balance provider schedules with patient needs.
Without command of these terms, schedulers risk inefficiency, revenue loss, and patient dissatisfaction.
Case Examples in Daily Practice
Consider a busy cardiology clinic managing high patient volumes. To reduce no-show rates, they implement automated text and call reminders, improving attendance by 25%. They also integrate real-time waitlists, filling cancellations within minutes and maintaining provider productivity.
In a pediatric practice, preauthorization protocols are essential for procedures like echocardiograms. Schedulers use EHR-integrated systems to confirm approvals before booking, avoiding revenue delays from insurance rejections.
A multi-provider family practice faces seasonal surges during flu season. They adopt a modified wave scheduling format, combining structure with adaptability, reducing patient wait times by 30% and increasing throughput.
An oncology clinic uses triage scheduling, ensuring urgent chemotherapy appointments receive priority. Their schedulers collaborate with clinical teams daily, adjusting appointments based on patient condition changes and lab results.
These examples highlight how terminology and practical application go hand in hand. Mastery of scheduling concepts empowers healthcare facilities to balance operational efficiency with patient care, elevating both satisfaction and revenue.
| Term | Definition |
|---|---|
| Time-blocking | Reserving specific periods for appointments to ensure smooth workflows and prevent overlaps. |
| Patient recall systems | Automated systems for follow-up scheduling, especially for preventive care or chronic management, integrated with EHRs. |
| Preauthorization requirements | Verification processes with payers to secure approval for procedures or specialist visits, avoiding claim denials. |
| Encounter types | Categories of appointments (e.g., new patient, established patient, procedure) that influence scheduling and billing. |
| No-show rates | The percentage of missed appointments, used to evaluate scheduling efficiency and the need for reminders or waitlists. |
| Waitlists | Lists of patients ready to fill cancelled slots, ensuring optimized provider utilization and reduced idle time. |
| Double booking | Scheduling multiple patients in the same slot, usually a last resort to handle high demand but risky for service quality. |
| Triage scheduling | Prioritizing appointments based on medical urgency, requiring collaboration with clinical teams for accurate assessments. |
| Capacity planning | Using historical data to forecast demand, balance resources, and optimize provider schedules for peak periods. |
Challenges in Medical Scheduling and Solutions
Overbooking and No-Shows
Medical schedulers face the dual challenge of overbooking and no-shows, each disrupting operations. Overbooking is often used to compensate for anticipated patient no-shows or last-minute cancellations. However, when all patients arrive, it creates bottlenecks, increased wait times, and provider stress. In practices with tight schedules, overbooking can push appointments beyond capacity, affecting quality of care and patient satisfaction.
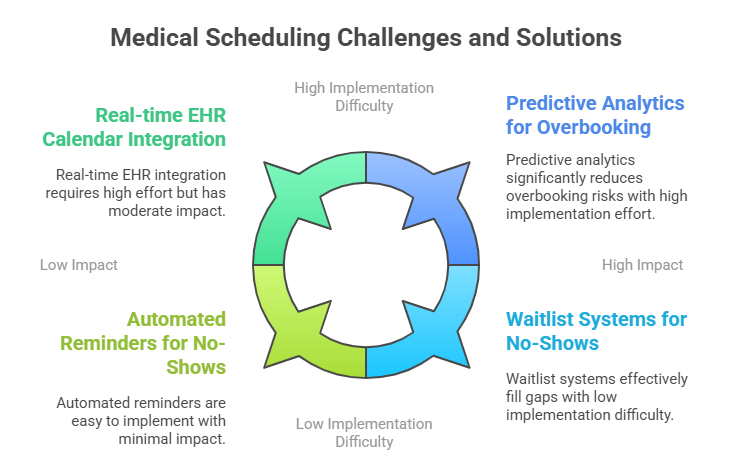
To mitigate this, clinics leverage predictive analytics tools that analyze historical data, no-show rates, and appointment types to optimize overbooking levels without risking overload. Integrating automated reminder systems, such as text and email notifications, significantly reduces no-shows, enhancing both patient engagement and clinic revenue.
No-shows result in lost revenue, idle provider time, and workflow disruptions. Proactive solutions include waitlist management systems, which fill last-minute gaps with patients awaiting earlier appointments. Clinics also adopt strict cancellation policies, requiring advance notice to discourage missed visits. Implementing these measures reduces no-show rates by up to 30%, improving operational stability.
Coordination with Providers
Effective scheduling hinges on seamless coordination with providers. Medical schedulers must align appointment slots with provider availability, considering factors like provider-specific appointment types, procedural times, and personal preferences. Disjointed communication can lead to double-bookings, appointment delays, or underutilized slots.
Schedulers utilize real-time calendar integrations within EHRs, providing instant visibility into provider schedules. These systems automatically flag conflicts and suggest alternate times, reducing manual errors. Provider-specific templates, outlining appointment durations, buffer times, and procedure requirements, ensure alignment with operational standards.
Regular collaboration meetings with providers help align scheduling strategies with clinical priorities. For instance, a provider may allocate specific days for new patients or procedures, while another focuses on follow-ups. Centralized communication systems, including shared dashboards or scheduling apps, maintain synchronization between front-desk teams and providers.
By streamlining communication and integrating technology, clinics minimize disruptions, maximize provider efficiency, and elevate patient satisfaction.
How Our Certification Prepares You For Medical Scheduling
Hands-On Training Highlights
Our Medical Scribe Certification by ACMSO—CPD-accredited and NHA-backed—equips premeds, pre-PAs, nursing, and high school students with advanced skills to master medical scheduling. This program doesn’t stop at surface-level knowledge; it delivers real-world proficiency through simulated EHR systems, HIPAA-compliant communication tools, and automated scheduling platforms. Students learn to handle SOAP notes, terminology, and over 90 clinical chief complaints with precision.
Training modules emphasize complex scheduling scenarios: managing multi-provider calendars, triage strategies, and capacity planning. Participants gain hands-on experience with EMR-integrated systems, ensuring accurate documentation and timely updates. Optional CMAA Administrative Assistant training covers billing, leadership, compliance, and office operations, giving graduates a competitive edge.
The curriculum includes live scenario workshops, where students practice dynamic scheduling challenges, refining both technical skills and decision-making. With real-time waitlist management, automated reminders, and scheduling strategies tailored to specialty areas—Ob/Gyn, Cardiology, Psychiatry, Emergency, Family Medicine—participants become adept at reducing no-show rates, enhancing clinic efficiency, and boosting revenue.
Medical Scribe Certification by ACMSO
Enrolling in the Medical Scribe Certification by ACMSO positions you for success in medical scheduling and beyond. Discover the full curriculum, explore specialty certification options, and register today by visiting our official course page. This comprehensive training provides the skills and confidence to thrive in dynamic clinical settings. Graduates emerge as versatile professionals, prepared to excel in high-pressure healthcare environments, balancing scheduling precision with patient-centered care.
Conclusion
Mastering medical scheduling is a cornerstone of efficient patient care and sustainable clinic operations. This field isn’t just about filling calendars—it’s about aligning complex workflows, minimizing errors, and elevating patient satisfaction. From reducing no-show rates through automated systems to managing dynamic multi-provider schedules, the ability to optimize appointment flows directly impacts both revenue and care quality.
The Medical Scribe Certification by ACMSO—CPD-accredited and NHA-backed—provides comprehensive training for premeds, pre-PAs, nursing students, and even high school learners. With in-depth modules covering SOAP notes, EMRs, HIPAA compliance, and over 90 clinical chief complaints, it offers hands-on mastery. Optional CMAA Administrative Assistant training extends capabilities to billing, leadership, compliance, and office operations, creating a well-rounded healthcare professional.
This guide has provided essential insights into medical scheduling, combining actionable strategies with practical examples. Whether you’re just entering the field or seeking to sharpen your expertise, the Medical Scribe Certification by ACMSO prepares you to handle real-world challenges with confidence. Take your scheduling skills—and career—to the next level by integrating knowledge with practice and standing out in today’s competitive healthcare landscape.
Frequently Asked Questions
-
Medical scheduling involves organizing patient appointments to align with provider availability, patient needs, and operational workflows. It ensures efficient clinic operations, reduces wait times, and improves patient satisfaction. Without precise scheduling, healthcare facilities face bottlenecks, underutilized resources, and revenue loss. Advanced tools like EHR integrations, automated reminders, and waitlist management enhance scheduling efficiency.
-
Overbooking aims to offset potential no-shows but can disrupt workflows when all patients arrive. It increases provider stress, prolongs wait times, and risks errors. Effective management involves predictive analytics, historical data review, and real-time calendar adjustments. The Medical Scribe Certification by ACMSO trains students to implement smart scheduling strategies, balancing appointment volume with resource availability while minimizing disruptions. Tools like automated reminders and strict cancellation policies also mitigate the negative effects of overbooking.
-
Medical offices use formats like stream scheduling, wave scheduling, and open-access scheduling. Stream scheduling assigns fixed time slots, wave scheduling groups patients, and open-access allows same-day or walk-in bookings. Modified wave scheduling blends these methods, providing balance and flexibility. Each format suits different clinical needs, patient volumes, and provider workflows. The Medical Scribe Certification by ACMSO covers these models in depth, offering hands-on practice in selecting and applying the right approach for specific healthcare settings.
-
Reducing no-show rates involves proactive strategies like automated text and email reminders, real-time waitlist management, and clear cancellation policies. Leveraging predictive analytics to identify high-risk no-show patients allows targeted outreach. The Medical Scribe Certification by ACMSO prepares learners to implement these tools, teaching them to monitor no-show metrics and adapt scheduling tactics accordingly. Successful clinics often see no-show reductions of 25–30% through these methods, improving provider utilization and revenue.
-
EHR systems provide real-time access to patient data, appointment statuses, and provider schedules. They enable seamless updates, reduce double-bookings, and ensure HIPAA-compliant communication. Integrated EHRs allow automated reminders, streamlined documentation, and synchronization between schedulers and providers. The Medical Scribe Certification by ACMSO trains students to navigate these systems expertly, ensuring accurate data handling and efficient scheduling processes in clinical environments.
-
The Medical Scribe Certification by ACMSO is a CPD-accredited, NHA-backed program tailored for premeds, pre-PAs, nursing, and high school students. It covers SOAP notes, EMRs, HIPAA compliance, and over 90 clinical chief complaints, equipping learners with comprehensive skills. Optional CMAA Administrative Assistant training expands competencies to billing, compliance, leadership, and office operations. Live scenario workshops and simulated environments prepare students to handle real-world scheduling challenges with confidence, ensuring readiness for dynamic healthcare roles.
-
Triage scheduling prioritizes patients based on medical urgency, ensuring critical cases receive immediate attention. It involves collaboration with clinical staff to assess symptoms and determine the appropriate appointment timing. Tools like EHR-integrated triage systems and communication dashboards support this process. The Medical Scribe Certification by ACMSO trains learners to implement triage strategies effectively, balancing patient needs with provider capacity while maintaining compliance and efficiency.