5 Surprising Skills You Gain as a Medical Scribe (Beyond Documentation)
Medical scribing starts as documentation, but the real payoff is what the job silently trains in you: decision support habits, pressure-proof communication, workflow instincts, and a quality mindset that most entry-level healthcare roles don’t teach. You sit inches away from clinical reasoning, watch how teams move when stakes spike, and learn how to turn chaos into a clean, defensible record. That combination compounds fast—and it’s why scribing often becomes a launchpad into higher-responsibility healthcare paths and why employers keep investing in the role (see medical scribe market trends and why facilities prefer certified scribes).
Below are 5 surprising skills you gain as a medical scribe beyond documentation—with practical ways to train them deliberately so you don’t just “do shifts,” you build career capital. This pairs naturally with the bigger trajectory captured in the medical scribe workforce report 2026–27 and how scribing stays relevant alongside tech in the AI-driven documentation future.
1. The 5 Skills Most Scribes Don’t Realize They’re Building (Until Later)
The best part about scribing is that the environment forces you to level up without asking permission. If you’re intentional, you’ll walk away with five skills that apply far beyond charting:
Clinical reasoning by proximity (pattern recognition, red flags, differential framing)
Systems thinking and workflow leverage (how care actually moves through a facility)
High-precision communication under pressure (clarifying fast, documenting neutrally, reducing friction)
Risk, quality, and audit discipline (what makes a note defensible and why accuracy becomes a safety tool)
Career-grade learning systems (how to absorb complex domains quickly, especially with evolving EHR/AI workflows)
These skills explain why scribes can meaningfully reduce provider load and burnout (see how scribes reduce physician burnout) and why facilities care about consistent, standardized performance (see documentation accuracy improvements and the annual documentation accuracy report).
A quick mindset shift: don’t treat your shift as “typing time.” Treat it as a repetition gym for clinical language, decision logic, and operational fluency—exactly the same way you’d train for certification using the medical scribe exam guide and sharpen gaps identified in the top scribe exam mistakes list.
Skill #1: Clinical Reasoning by Proximity (You Learn the “Why,” Not Just the “What”)
Scribes absorb clinical reasoning the way apprentices absorb craft: by seeing the decision process repeated across hundreds of cases. Over time, you stop hearing “order CT” as a command and start hearing the logic underneath it—rule out bleeding, evaluate obstruction, confirm pneumonia, stratify risk. That’s a rare advantage early in a healthcare career, and it’s one reason scribing stays valuable even as technology evolves (see the AI-driven documentation landscape).
Here’s how this skill actually forms:
You learn red flags as narrative triggers. When a provider’s tone changes—sudden chest pain, neuro deficits, high-risk meds—you learn what details must be captured immediately. That habit becomes a quality superpower, and it aligns with the measurable accuracy gains discussed in how scribes improve documentation accuracy and the annual documentation accuracy report.
You learn how to build a defensible timeline. A strong HPI isn’t “long.” It’s chronological and decision-ready. That same timeline discipline is what makes ED course notes readable in fast settings and reduces follow-up edits—an efficiency outcome tied to burnout reduction in this physician burnout report.
You learn the difference between symptoms and clinical meaning. “Dizzy” can mean dehydration, stroke, arrhythmia, medication effect, or anxiety. As a scribe, you learn how providers disambiguate with targeted questions—then you learn to capture those questions and answers cleanly, using correct clinical language reinforced by medical terminology mastery.
How to train this deliberately (not passively):
After each patient, write a one-sentence “why the plan makes sense” summary (for yourself, not in the chart). It forces you to notice the logic chain—chief complaint → risks → differential → tests → interpretation → disposition. That’s the exact mindset that helps you perform better in standardized training pathways like the scribe certification exam guide, and it’s the same way high performers avoid errors highlighted in top scribe exam mistakes.
2. Skill #2: Systems Thinking and Workflow Leverage (You Learn How Healthcare Actually Moves)
Most people think healthcare is “doctor sees patient, writes note.” In reality, care is a flow system—triage, orders, results, consults, documentation, discharge planning, and follow-up logistics. Scribes sit at the intersection of that flow and learn something priceless: where bottlenecks form, what causes rework, and how small documentation choices either accelerate throughput or slow everything down.
This is why scribing builds operational intuition that transfers to roles in administration, care coordination, analytics, and leadership—and why the demand picture keeps expanding in reports like the medical scribe workforce report 2026–27 and the job growth analysis nationwide.
What systems thinking looks like on shift
You document in the order that prevents follow-up questions. A note that anticipates coder, nurse, or consultant needs reduces back-and-forth—exactly the kind of downstream efficiency tied to hospital revenue impact.
You learn patient flow as a language. “Roomed,” “boarded,” “dispo pending,” “consult placed,” “awaiting imaging” aren’t just statuses—they’re signals. If you want to build vocabulary that matches real workflow systems, use resources like patient flow management terms and patient management systems terms.
You understand why clarity matters more than length. A short, clear ED course entry that shows “result → action → reassessment” is higher value than a paragraph of noise. That clarity supports the accuracy outcomes in documentation accuracy by 90%+ and helps keep providers out of after-hours editing spirals highlighted in burnout reduction insights.
The surprising part: workflow leverage makes you “feel” like a clinician
Not because you diagnose—but because you understand the operational consequences of clinical decisions. You learn which details unlock safe discharge, which details justify admission, and which missing fields cause delays. That’s exactly why facilities value standardized scribing (see why facilities prefer certified scribes) and why the market remains strong in future job trend coverage.
3. Skill #3: High-Precision Communication Under Pressure (The “Real” Soft Skill)
Scribes quickly learn that communication isn’t a personality trait—it’s a safety tool. In fast settings, the ability to clarify a detail once (and document it correctly) prevents hours of rework later. This is why scribes become trusted: not because they talk a lot, but because they communicate cleanly.
Here’s the core of pressure-proof scribe communication:
1) You learn how to ask “one good question” instead of ten weak ones
Strong scribes ask for load-bearing details only:
onset/time course,
laterality/site,
dose/frequency,
who was consulted and what they recommended,
what changed the plan.
That discipline is the same mental model that improves performance on the certification path laid out in the scribe exam guide and reduces errors called out in the top exam mistakes guide.
2) You learn neutral documentation language that reduces conflict
When situations get tense, scribes learn to document observed facts instead of interpretations. That’s not just professionalism—it’s risk protection. Pair this with communication fundamentals from active listening scenarios and real-world communication standards like telephone etiquette, because healthcare communication often happens across calls, messages, and quick hallway updates.
3) You learn how to build trust by reducing friction
When your notes consistently reflect reality—without missing key facts—providers stop re-reading your work. That trust compounds into more autonomy, better learning access, and stronger references. It’s also the mechanism behind measurable outcomes like higher accuracy (see how scribes improve accuracy) and reduced burnout from fewer after-hours corrections (see burnout report).
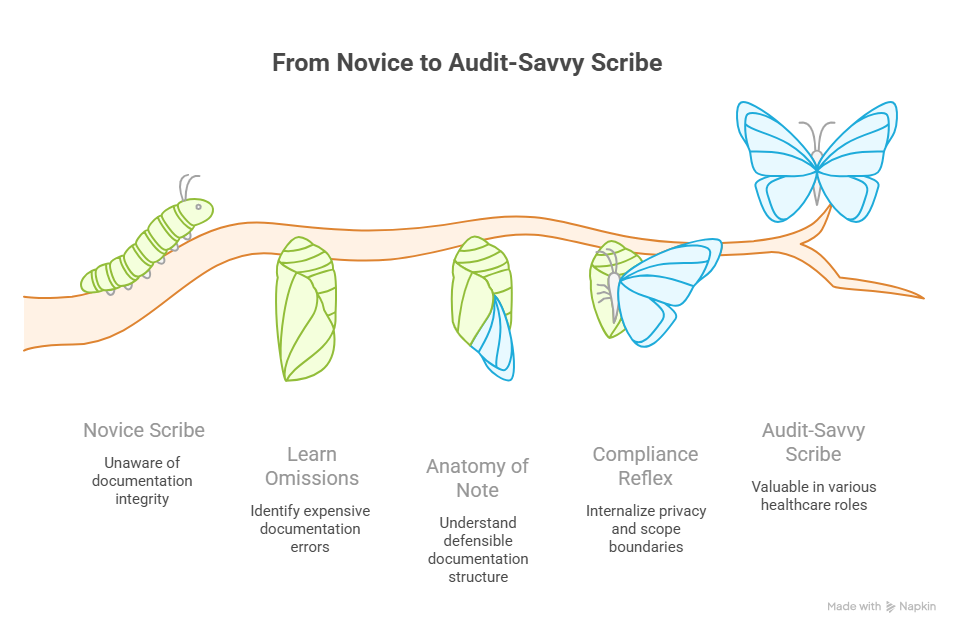
4. Skill #4: Risk, Quality, and Audit Discipline (You Learn What Makes a Record Defensible)
This is the skill most people never learn until something goes wrong: healthcare runs on documentation integrity. A record can be clinically correct and still be operationally weak if it’s missing the elements that prove decision-making, consent, reassessment, and disposition safety. Scribes become unusually fluent in that hidden layer.
How audit discipline forms in scribes
You learn which omissions are “expensive later.” Missing laterality, missing time-based reassessment, unclear consult notes, vague procedures—these trigger coder queries, denials, and risk reviews. This connects directly to revenue outcomes discussed in hospital revenue impact analysis.
You learn the anatomy of a defensible note. Not long—defensible: clear timeline, clear reasoning, clear response to interventions, and clear disposition logic. That’s the same standard behind the annual documentation accuracy report and why facilities prefer structured performance (see certified scribe preference).
You learn compliance boundaries as a professional reflex. Privacy and scope matter. If you’re not anchored here, read HIPAA simplified and keep your documentation rooted in what was stated and done—not what you assume.
Why this becomes a career advantage
Audit discipline is portable. It makes you valuable in:
clinical operations,
quality improvement,
utilization management,
coding-adjacent workflows,
healthcare administration roles.
And it keeps paying off as remote and AI workflows expand (see remote scribe market growth and the AI-driven documentation future).
5. Skill #5: Career-Grade Learning Systems (How Scribes Become Fast Learners in Complex Environments)
Scribing quietly turns you into a fast learner because you’re forced to:
absorb new terminology daily,
adapt to provider styles,
navigate EHR workflows,
stay accurate under interruptions,
continuously correct small gaps.
That’s not “experience.” That’s a learning system forming.
The three learning systems scribes accidentally build
1) Context-based vocabulary acquisition
You don’t memorize terms in isolation—you learn them attached to symptoms, plans, and outcomes. Reinforce it with the medical terminology quick study guide.
2) Feedback loops
Provider edits teach you instantly what matters. Track edits (what changed and why) and you’ll improve faster than almost anyone. This is also why certification prep becomes easier over time (see essential study techniques and the interactive practice exam).
3) Standardization under change
Scribes learn to operate in evolving systems—new EHR features, new templates, new compliance expectations. That adaptability is exactly what keeps the role strong in market reports like employment trends visualization and the annual employment report.
How to turn these skills into promotions or better roles
Document your skill growth like a professional:
“Reduced provider edits by X%”
“Improved note closure time”
“Lowered coder query frequency”
“Built standardized templates/macros”
“Handled high-volume shifts with stable accuracy”
That evidence maps directly to employer expectations in facility preference for certified scribes and to the hiring momentum shown in market trends.
6. FAQs: 5 Surprising Skills You Gain as a Medical Scribe (Beyond Documentation)
-
Clinical reasoning by proximity. You repeatedly witness how providers think, test, and decide. Over time, you learn the logic patterns that drive safe care—especially when you focus on accuracy frameworks like documentation accuracy improvements.
-
Use measurable signals: fewer edits, faster closures, stronger note completeness, lower coder queries, and better handoff-ready documentation. These tie directly to operational outcomes discussed in hospital revenue impact and burnout reduction outcomes in this report.
-
Yes—especially timeline control, communication clarity, and audit discipline. Remote environments punish ambiguity, which is why market demand continues to expand (see remote market growth).
-
AI can draft text, but it still struggles with chaotic context, subtle decision pivots, and “what actually happened.” Your value becomes verification, structure, and integrity—exactly the direction explained in how scribes fit into an AI-driven world.
-
Start with terminology and documentation structure, then add exam-focused discipline:
-
Because standardization reduces risk, improves consistency, and lowers rework. That preference is spelled out in why facilities prefer certified scribes and reflected in hiring patterns across market trends.
-
Be consistently accurate, neutral, and timeline-clean. Ask only load-bearing clarifications, and keep your documentation defensible. Over time, that trust becomes access—better learning exposure, more responsibility, and stronger career momentum documented in workforce insights like the scribe workforce report 2026–27.