Surgical Scribing 101: Essential Techniques & Best Practices
Surgery is where documentation has the least forgiveness. The room is sterile, the tempo is relentless, the vocabulary is precise, and the record must support patient safety, continuity, coding, quality reporting, and medicolegal defensibility—all while the team is focused on the operative field. Surgical scribing isn’t “note-taking.” It’s structured capture of indications, intraoperative decision-making, procedure steps, implants, counts, specimens, complications, and postoperative plans in a way that survives audits and handoffs.
This guide teaches you the practical techniques that make you useful on day one: how to build a pre-op charting scaffold, how to capture the operative narrative without guessing, and how to document like a system so nothing critical disappears in the blur of a busy list.
1. Surgical Scribing Fundamentals: What Makes OR Documentation Different From Every Other Setting
Surgical documentation has two realities you must respect: time compression and precision demand. A clinic note can be clarified later. A surgical case often cannot. The operative record is expected to be complete, chronological, and consistent with what actually happened—down to laterality, approach, devices, and the rationale for deviations from plan. That is exactly why facilities prefer trained, standardized scribes: fewer errors, faster productivity, and more consistent notes (see why healthcare facilities prefer certified medical scribes).
The four “outputs” your documentation must support
Surgical notes exist for:
Clinical continuity (post-op care, complications, future procedures)
Coding & billing (CPT/ICD alignment, supplies, modifiers, device billing)
Quality & compliance (timeouts, counts, antibiotic timing, VTE prophylaxis where documented)
Risk defense (clear indication, consent, technique, complications, disposition)
Scribing mastery means knowing what information is load-bearing—the details that, if missing, create downstream failure. If you want to understand how documentation quality scales across environments, anchor to the principles in how scribes improve documentation accuracy by over 90% and the operational impact outlined in the annual report on clinical documentation accuracy.
What you never do in surgical scribing
In surgery, guessing is lethal to quality. You do not:
invent steps you didn’t observe,
“clean up” language by changing meaning,
infer implant sizes or device names,
document complications you didn’t hear stated,
add times unless captured from the record/workflow.
Your value comes from being a high-reliability recorder of what was actually done and what was actually decided. If you’re building long-term career credibility, treat this like certification discipline (see complete guide to passing your medical scribe certification exam and top 10 medical scribe exam mistakes).
Surgical scribing is a workflow role, not a passive role
High-performing surgical scribes actively reduce friction by preparing documentation scaffolds before incision and keeping a tight intraop timeline, while staying within compliance boundaries (ground your privacy and access basics in HIPAA simplified). When you can consistently produce notes that need fewer edits, you directly reduce cognitive load and charting hours—exactly the mechanism described in how medical scribes reduce physician burnout.
2. Surgical Scribing Mistakes That Trigger Audits, Denials, and Rework (And How to Prevent Them)
This is the part of surgical scribing nobody warns you about: most “mistakes” aren’t dramatic—they’re quiet omissions that only become expensive later. The fastest way to get pulled into chart rework (or worse, an audit trail) is inconsistent laterality, vague procedure naming, and device documentation that doesn’t match what was actually used. Build a hard rule: if the case has a side, the side must appear in the header, time-out reference (if documented), and technique narrative—the same way. One mismatch forces downstream clarification and kills efficiency, which is exactly why facilities invest in standardization and credentialed workflows (see why healthcare facilities prefer certified medical scribes). Another common trigger is “template bloat”: copying generic technique text that doesn’t reflect the actual case. That creates internal contradictions providers must fix later—fuel for after-hours charting and burnout (supported by the patterns in how medical scribes reduce physician burnout).
The OR’s highest-risk omission cluster is implants/devices + specimens + counts. If any one of those is incomplete, you create traceability issues, coding delays, and sometimes compliance escalations. Treat device capture as a verification process, not a memory game: align your note with what the system shows and what the team confirms, and keep your EHR navigation sharp using EMR software terms. Missing “decision pivots” are another silent failure: if an unexpected finding changes the approach, your operative narrative must show what was found and why the plan changed—otherwise the note looks like a gap in reasoning, not clinical judgment. This level of clarity is directly tied to measurable documentation quality outcomes like those discussed in how scribes improve documentation accuracy by over 90% and the broader standards in the annual documentation accuracy report.
Finally, don’t underestimate “soft failures” that become compliance problems: documenting beyond scope, adding assumptions, or drifting into non-neutral language during tense moments. Stay grounded in privacy and access basics via HIPAA simplified, and use structured communication habits from active listening scenarios and conflict resolution guidance to clarify fast without disrupting flow. If you want a practical self-audit loop, study failure patterns from top 10 medical scribe exam mistakes, reinforce fundamentals in the scribe certification guide, and remember: clean notes don’t just protect patients—they protect revenue and throughput, exactly as shown in how scribes impact hospital revenue.
3. Pre-Op, Intra-Op, Post-Op: The Surgical Scribe Workflow That Prevents Missed Details
Surgical scribing becomes predictable when you treat every case as a three-act structure. Each act has must-capture items and high-risk failure points. Your job is to build a documentation system that works even when the room gets chaotic.
Act 1: Pre-op documentation scaffold (before the patient is draped)
This is where elite scribes quietly win. Before incision, you should have:
procedure name(s) + laterality,
indication and brief clinical background,
planned approach and key anticipated steps,
consent status (as documented),
relevant allergies/risks,
equipment/implant expectations (when applicable).
If you’re not fluent in EHR navigation, you will fall behind here; tighten your EHR vocabulary using EMR software terms walkthrough and operational workflow basics like patient management systems. This preparation is the difference between capturing the procedure accurately and trying to reconstruct it after the fact.
Act 2: Intra-op capture (the operative narrative as a controlled timeline)
Intra-op scribing is about chronology without clutter. You are capturing:
key steps (high-level, correct order),
findings that explain decisions,
devices/implants actually used,
events (bleeding control, complications, conversions),
counts and safety confirmations (as documented),
specimen handling.
The hardest part is decision pivots. When surgeons adapt mid-case, your note must show:
what new information appeared (finding),
what changed in technique (decision),
what safety actions were taken (hemostasis, consult, conversion, termination rationale).
This is where scribes protect revenue and reduce rework: a clean operative narrative reduces coder queries and prevents the “chart ping-pong” that adds hours to a surgeon’s day (the broader operational impact is connected to revenue in how scribes impact hospital revenue and to workload in burnout reduction).
Act 3: Post-op clarity (what happens next must be obvious)
Post-op documentation is where downstream care succeeds or fails. Your note should make it easy for PACU, floor teams, and follow-up clinicians to know:
what was done,
what was found,
what changed from plan (if anything),
what devices/drains are present,
what the immediate plan is (pain, diet/activity, antibiotics, follow-up).
Think of this as the “handoff contract.” Weak post-op plans lead to phone calls, confusion, and delays. Strong plans reduce friction across the system—especially in hybrid/remote documentation models described in remote medical scribe market growth.
4 . Technique Without Guessing: How to Document Operative Steps Accurately Under Pressure
The best surgical scribes write notes that feel “inevitable”—as if the procedure could only have been documented that way. That comes from controlled phrasing and disciplined observation.
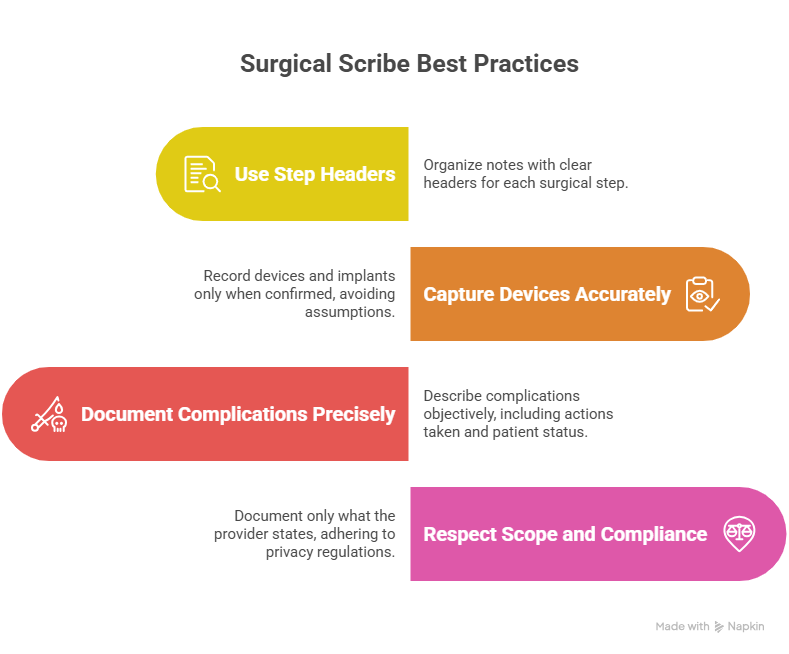
Use “step headers” instead of narrative sprawl
When the procedure is complex, narrative paragraphs collapse. Use step headers:
Exposure
Dissection
Resection/repair
Hemostasis
Closure
Disposition
Under each header, capture only what was actually performed and stated. This keeps your note audit-friendly and readable. It also makes it easier for surgeons to review quickly—reducing edits and improving same-day completion (a core operational KPI discussed across workforce materials like employment trends).
Capture devices and implants as they are confirmed
Device documentation fails in two ways: missing detail or wrong detail. Your rule:
record the device/implant once it is verbally confirmed or visibly documented in the system,
never “fill in the blank” based on what’s typical,
use the implant log when available rather than memory.
Document complications with calm precision
If a complication occurs, your note should include:
what happened (objective),
what was done (management),
patient status (stable/condition),
outcome at the end of case.
Avoid emotional tone; keep it clinical. This protects the patient and the team by keeping the record clear.
Respect scope and compliance boundaries
Scribes document; they don’t order, diagnose, or decide. If you’re unclear where boundaries sit in your environment, keep your language anchored to what the provider states and use privacy fundamentals from HIPAA simplified. Consistent scope discipline is a major trust signal for surgical teams.
5. Best Practices That Make Surgical Scribes “Indispensable” (Speed, Accuracy, Trust)
Surgical scribing is not about being invisible. It’s about being reliably useful without disrupting the room. Here are the best practices that get you trusted fast.
1) Create a “case blueprint” before incision
A blueprint is a one-page mental map of:
indication,
procedure name(s),
laterality,
approach,
expected equipment/implant needs,
“watch items” (anticipated complication risks).
Blueprints prevent missed detail when the surgeon moves quickly through standard steps. This is a repeatable performance system—exactly what hiring teams look for in high-demand markets (see market trends and where jobs will be and broader workforce outlooks like the annual employment report).
2) Keep the narrative “short, structured, and defensible”
Your note should never read like a transcript. It should read like a clinical record:
minimal fluff,
maximal clarity,
no contradictions.
3) Build a surgeon-specific template library (without template laziness)
Templates are good when they prevent omissions, not when they paste generic language. Use templates that force critical fields:
laterality,
approach,
findings,
implants,
specimens,
counts,
complications,
disposition.
This is the same principle behind performance improvements in documentation accuracy (see documentation accuracy report).
4) Treat “counts, specimens, implants” as a triple-lock system
These three categories cause disproportionate risk when wrong. Your triple-lock system:
capture when verbally confirmed,
verify in the record where available,
ensure the operative note reflects what the system shows.
5) Communicate like a pro when clarification is needed
In the OR, you can’t ask constant questions. But you also can’t leave critical ambiguity. Use short, timing-respectful clarifications and be excellent at listening. If you want to sharpen that skill, use active listening scenarios and professional communication standards like telephone etiquette (because post-op coordination and surgical follow-ups often rely on clean communication and accurate documentation).
6) Future-proof: learn how surgery documentation evolves with AI
Surgery will adopt AI drafting, but accuracy will still depend on humans who can:
validate what happened,
capture deviations and decision pivots,
ensure device traceability,
maintain defensibility.
This future-forward view is captured in how scribes fit into AI-driven documentation, and it’s one reason surgical scribing remains a strong pathway in the evolving medical documentation ecosystem.
6. FAQs: Surgical Scribing 101 — Essential Techniques & Best Practices
-
The indication + what was actually done + what was found + what changed + what’s next. If any one of those is missing, the note becomes weak for continuity, coding, and risk defense.
-
Use a structured high-level step framework (exposure → key maneuver → repair/resection → hemostasis → closure) and only record steps that are stated or clearly observed. Templates help only if they force critical fields rather than paste generic filler.
-
Laterality inconsistencies, missing approach clarity, undocumented implants/devices, unclear complexity rationale, and missing specimen documentation. Tight capture reduces the chart ping-pong that burns time and contributes to after-hours work (see burnout reduction report).
-
Record them when confirmed, don’t infer sizes/models, and ensure the op note aligns with the implant log or documented device record when available. Device traceability is not optional; it’s a patient safety and billing requirement.
-
State what occurred, what action was taken, and the status at the end of the case—calm, objective, and chronological. Avoid speculation and emotional tone.
-
Yes—because precision documentation remains valuable even as AI expands. Hiring demand continues to follow standardized skill signals (see facility preference for certified scribes and macro hiring patterns in market trends).
-
Terminology fluency + structured documentation + compliance boundaries. Use the certification track as your backbone: certification exam guide, stress-test with the practice exam, and eliminate errors using top exam mistakes.