Medical Office Automation Trends: Opportunities for CMAAs
Medical office automation is not a futuristic idea. It is already reshaping how front desks run, how documentation moves, and how revenue gets protected. The CMAAs who win in this shift are the ones who understand workflows, control compliance, and become the person who can translate automation into real clinic outcomes. This guide breaks down the most important automation trends, the highest ROI opportunities, and the exact skills that keep you indispensable, aligned with telehealth expansion changes and the compliance reality in HIPAA updates for 2025.
1) What Automation Really Means Inside a Medical Office Today
Automation is not one tool. It is the redesign of how work moves through a clinic. The biggest shift is that “busy work” is being replaced by systems that route tasks, validate data, and trigger actions without a human pushing every step. That includes everything from intake and scheduling to claims and follow ups. The clinics adopting this fastest are the ones under pressure from staffing shortages, rising patient volume, and stricter documentation expectations, all highlighted in healthcare documentation trends and the workflow discipline behind efficient EMR data entry.
CMAAs often assume automation threatens their job. In reality, it threatens unstructured tasks. It rewards professionals who can run standardized processes, maintain privacy controls, and prevent revenue leakage. If you can identify what should be automated, what must stay human, and what must be documented, you become the operational anchor. That value shows up in market demand signals like major providers increasing hiring of certified medical admin assistants and how workflows are changing under telemedicine’s growing need for medical scribes.
The core trend is that automation is moving upstream. Clinics are automating the earliest touchpoints because that is where errors start. Bad intake data becomes downstream chaos. Wrong insurance info becomes denied claims. Weak privacy handling becomes risk. If you understand intake structure and quality control, you will see automation as leverage, not replacement. That skill overlaps heavily with the audit mindset in mastering patient chart audits in EMR systems and the protection mindset in EMR security best practices.
Another major trend is that automation is being bundled with AI driven assistance. That does not mean clinics want robots doing everything. It means they want better routing, faster summarization, and fewer repetitive clicks. This is the same direction described in automation and AI reshaping medical roles and it connects directly to the administrative side through billing basics for CMAAs. CMAAs who can supervise these systems become the ones clinics trust with operations.
2) The Highest Value Automation Opportunities for CMAAs
CMAAs should aim for automation that reduces errors, protects revenue, and improves patient experience without creating compliance risk. The highest ROI is often in the middle of the workflow, where tasks get dropped and where staff rely on memory. When you automate those weak points, you reduce chaos and improve outcomes. This is exactly why clinics emphasize structured operations in essential daily office checklists and why quality control is tied to chart audit readiness.
One major opportunity is intake plus eligibility verification. If the clinic is automating reminders but still manually fixing missing insurance fields, it is automating the wrong layer. Eligibility errors turn into denial rework and uncomfortable patient billing conversations. CMAAs who can build a clean intake flow and verification checkpoints become the person leadership relies on. This ties directly into revenue protection patterns explained in medical billing basics for CMAAs and the avoidable failures highlighted in top medical billing errors CMAAs must avoid.
Another high value area is EMR task routing. Most clinics have hidden task debt. Messages sit. Results sit. Prior auth requests sit. If you can help implement event based tasks and escalation rules, you eliminate silent failures. This is the administrative mirror of the discipline in efficient EMR data entry workflows and it protects patient safety in the same way documentation discipline supports clinical efficiency improvements.
Telehealth is also accelerating automation. Telehealth intake can be automated with device checks, identity confirmation prompts, consent capture, and pre visit questionnaires. This reduces failed visits and reduces time wasted on basic troubleshooting. The best CMAAs position themselves as telehealth workflow owners because these processes touch compliance, scheduling, and documentation at the same time. Build your thinking around telehealth expansion and the broader workforce signals from telemedicine’s growing need for medical scribes.
A final high value opportunity is compliance automation that strengthens controls. This includes access monitoring, audit logs, secure document routing, and standardized privacy messaging. Automation can reduce human error, but only if you design it correctly. You anchor this work in HIPAA compliance essentials, reinforce it with navigating patient privacy regulations, and protect it with EMR security best practices.
3) The Skills CMAAs Must Build to Lead Automation Instead of Fearing It
Automation rewards CMAAs who become process thinkers. Clinics do not need someone who can click faster. They need someone who can map workflows, reduce errors, and enforce compliance standards. This is why training resources increasingly emphasize standardized thinking like OSHA compliance steps and why privacy remains non negotiable in HIPAA updates for 2025.
The first skill is workflow mapping. You must be able to describe the process in steps, identify where it breaks, and define what an automated trigger should do. This is the same mental model used in efficient EMR entry and in quality control practices from patient chart audits. When you can map workflows, you can supervise automation without being confused by it.
The second skill is data quality discipline. Automation amplifies whatever data you feed it. Bad data becomes fast bad outcomes. You need to care about required fields, standard naming, and clean documentation inputs. This connects to the structured approach in ICD 10 coding simplified and to basic revenue integrity from billing basics for CMAAs.
The third skill is compliance judgment. Automation cannot replace human responsibility for privacy and security. You need to understand who can access what, when consent is required, and how information is transmitted. Ground your decision making in HIPAA compliance essentials, reinforce scenarios with patient privacy best practices, and protect workflows through EMR security best practices.
The fourth skill is change management. Automation fails when staff do not adopt it. Your role is to make the process easier, not just different. That means creating training checklists, defining exception handling, and building escalation paths. Your best blueprint is the systems mindset behind essential daily office procedures and the operational clarity seen in office inventory management. If you can make adoption smooth, you become the person leadership trusts with every new tool.
4) The CMAA Automation Playbook: How to Adopt Tools Without Breaking Compliance
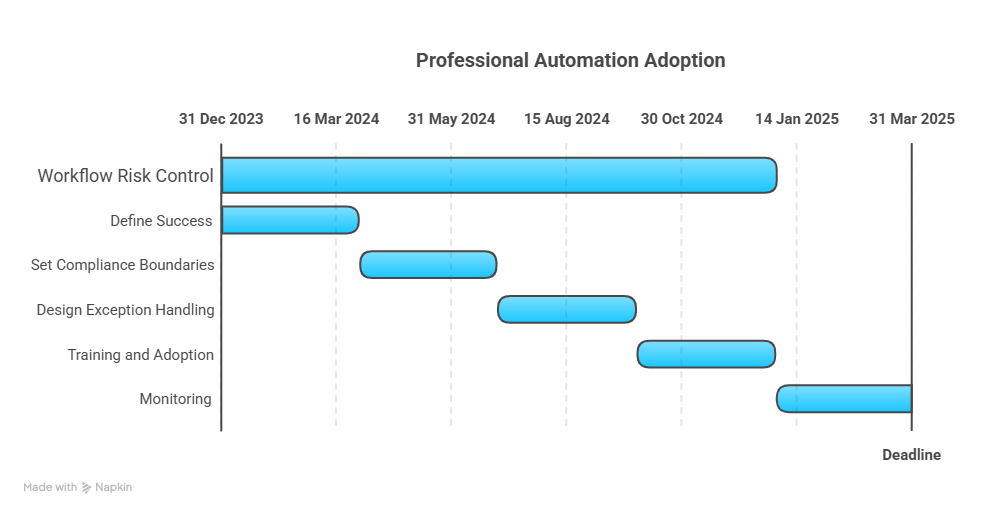
Professional automation adoption starts with workflow risk control. The fastest way to fail is to implement a tool and hope staff figures it out. A CMAA led playbook should always include scope, process, exceptions, training, and monitoring.
Step one is to define what success looks like in measurable terms. Examples include fewer no shows, fewer eligibility errors, faster message routing, or fewer denials. This aligns automation with business outcomes. It also prevents “tool collecting” that creates chaos. Use operational thinking inspired by daily office procedure checklists and quality controls used in chart audits.
Step two is to set compliance boundaries before you automate. Identify what data the tool touches, how it stores it, and who can access it. If you cannot clearly explain those answers, the workflow is unsafe. Anchor your rules in HIPAA compliance essentials, strengthen your scenario thinking with patient privacy best practices, and enforce technical discipline through EMR security best practices.
Step three is to design exception handling. Automation should handle the standard path, but humans must own edge cases. Your exception rules should be specific. If insurance eligibility fails, what happens next. If a patient replies “stop” to reminders, what happens next. If a portal message is urgent, what happens next. This process thinking is the same discipline that protects performance in high volume environments influenced by telehealth expansion and the operational strain described in major providers increasing CMAA hiring.
Step four is training and adoption. Staff do not need long training. They need clarity and repetition. Build a one page process guide, a short checklist, and a weekly review loop for the first month. For inventory, use structured routines like office inventory management. For compliance training, reinforce operational expectations from OSHA compliance steps and privacy rules from HIPAA updates for 2025.
Step five is monitoring. Automation must be audited. Track failure rates, patient complaints, denial reasons, and staff feedback. This mindset overlaps strongly with audit readiness from patient chart audits and it protects against silent errors the same way secure operations are reinforced in EMR security best practices.
5) Career Upside: How Automation Expands CMAA Roles and Pay Leverage
Automation creates winners and losers. The winners are the CMAAs who become workflow owners. Clinics will always need humans who can coordinate teams, protect compliance, and ensure systems actually work in reality. That is why hiring signals keep rising, as shown in major providers increasing certified CMAA hiring and why policy changes like CMS billing code updates increase the need for operational control.
If you can speak the language of billing risk, you become more valuable immediately. Automation often touches coding prompts, claim submission checks, and denial queues. You do not need to be a coder, but you must understand where errors originate and how to stop them. Build that foundation using medical billing basics for CMAAs, reinforce accuracy through ICD 10 coding simplified, and avoid costly habits outlined in top billing errors CMAAs must avoid.
Automation also creates new specialties inside admin teams. You can move into roles like operations coordinator, compliance assistant, scheduling optimization lead, or EMR workflow specialist. These roles expand further as care models shift through telehealth expansion and privacy requirements evolve with HIPAA updates for 2025.
If you want geographic leverage, target markets with strong healthcare growth and system adoption. Use region specific insights like Texas medical admin assistant opportunities and workforce patterns like why Chicago hospitals are hiring more CMAAs. These pages are not just content. They are signals about where demand, pay, and automation adoption are moving.
Your biggest career move is to stop positioning yourself as someone who “does tasks” and start positioning yourself as someone who “runs workflows.” Automation does not remove the need for leadership. It exposes the need for it.
6) FAQs: Medical Office Automation Trends for CMAAs
-
Automation replaces repetitive actions, not professional judgment. Clinics still need humans to manage exceptions, protect privacy, and coordinate patient workflows. If you become the person who understands compliance boundaries in HIPAA compliance essentials and security controls in EMR security best practices, you become harder to replace, not easier. The opportunity is to own workflows, not to cling to busy work.
-
Start with reminders, intake cleanup, or task routing for non urgent processes. These improve efficiency quickly while keeping risk manageable. Use operational structure from essential daily office procedures and align intake workflows with efficient EMR data entry. Avoid automating anything that touches PHI until privacy and access rules are clearly defined.
-
Watch for unauthorized access, incorrect recipients for messages, weak consent capture, and insecure document routing. These risks become more complex as operations expand with telehealth changes. Anchor your boundaries in patient privacy best practices and strengthen your readiness with HIPAA updates for 2025.
-
Automation can prevent denials by validating eligibility, catching missing fields, and routing prior auth tasks with deadlines. The key is pairing automation with review. Build your foundation from medical billing basics for CMAAs, reduce risk using top billing errors, and stay aligned with policy shifts like CMS billing code changes.
-
Learn workflow mapping, data quality, compliance judgment, and change management. Practice by building simple checklists and escalation rules based on daily procedures and audit discipline from chart audits. Pair privacy discipline from HIPAA compliance essentials with security thinking from EMR security best practices.
-
Track measurable improvements: reduced no shows, faster message routing, fewer denials, fewer intake errors, and smoother telehealth visits. Then document your role in designing and enforcing the process. Tie your work to compliance readiness using OSHA compliance steps and privacy clarity through HIPAA updates for 2025. Clinics promote people who create stability, not just activity.