Efficient Medical Office Management: Essential CMAA Skills
Efficient medical offices don't run on chance — they run on high-functioning Certified Medical Administrative Assistants (CMAAs). These professionals are the backbone of every successful clinic, bridging the gap between patient care and operational control. As front-line coordinators, CMAAs influence wait times, patient satisfaction, and even billing accuracy. In 2025, clinics face rising patient loads, tighter regulations, and tech-heavy workflows. Without skilled CMAAs, daily chaos becomes inevitable.
This guide breaks down exactly what CMAAs must know to operate at peak performance — and how our CMAA certification program trains you in real-life medical office conditions, not generic theory. From intake and scheduling to HIPAA and billing, we cover the skills that save time, prevent errors, and make CMAAs irreplaceable.
Core Administrative Responsibilities
Patient Intake Management
The first point of contact in any medical office determines everything that follows. CMAAs are responsible for streamlining the intake process so that clinicians can focus purely on care. This includes collecting accurate patient demographics, verifying insurance, and ensuring consent forms are completed before the appointment begins.
Errors in this stage can lead to denied claims, misfiled records, or compliance breaches. That’s why CMAAs must:
Cross-check patient names, DOB, and insurance ID numbers
Ensure HIPAA acknowledgment forms are signed and stored
Use standardized language when confirming information verbally
Flag missing information in real time to avoid delays
Efficient intake isn’t about rushing — it’s about having repeatable systems that work under pressure and across dozens of appointments per day.
Appointment Scheduling Protocols
Scheduling isn’t just about filling slots — it’s about balancing provider availability, patient urgency, and insurance requirements. CMAAs must be fluent in both manual and automated scheduling tools, understanding when to override systems and how to manage double-bookings or urgent walk-ins without disrupting flow.
Key elements include:
Using ICD-10/CPT data to match appointments with billing codes
Recognizing pre-authorization requirements and scheduling around them
Flagging time blocks for certain procedures or recurring patients
Maintaining follow-up reminders and cancellation logs
When done well, scheduling can increase patient throughput by 25%, improve wait times, and reduce no-show rates — all while protecting staff sanity.
Electronic Health Record Accuracy
EHR misentries are a top cause of compliance penalties and patient risk. CMAAs must not only navigate complex EHR systems but also maintain zero-tolerance for data ambiguity.
High-efficiency CMAAs do the following:
Log physician notes with standardized modifiers and no typos
Accurately record insurance and copay details under the right fields
Ensure continuity of care documentation across provider networks
Use time-stamps and audit trails to maintain record integrity
With multiple stakeholders relying on the same patient chart, accuracy isn't optional — it's mandatory. This is why our CMAA certification includes hands-on training with live EHR simulations used in actual medical facilities.
Communication and Front Desk Etiquette
Tone and Language for Patient Calls
In a clinical setting, every phone call is a reflection of the practice’s professionalism. CMAAs must consistently use calm, concise, and empathetic language — whether speaking with a first-time patient or a frustrated return caller. A single misworded phrase can escalate tension or result in a poor online review that damages patient trust.
Essential call handling skills include:
Greeting with a standardized, HIPAA-compliant intro
Avoiding jargon and using clear patient-first language
Summarizing information before ending the call to avoid confusion
Always confirming appointment times, dates, and any prep requirements
CMAAs must also know how to de-escalate frustrated patients by validating their concerns, avoiding blame language, and offering precise next steps. This soft skill, when mastered, is a retention booster in high-volume practices.
Handling Escalations Professionally
Escalations aren’t always avoidable — but how they’re handled defines the office culture. CMAAs are often the first to hear complaints about wait times, billing disputes, or denied referrals. What separates top-tier administrative staff is their ability to manage the issue without emotion and route it efficiently to the right internal party.
A professional escalation response includes:
Active listening without interruption
Using neutral phrases like “Let me make sure I understand your concern…”
Logging the complaint formally and time-stamping it
Escalating to clinical, billing, or management based on content
Practices with clear escalation protocols see faster resolution times and improved staff morale. In our CMAA certification training, students learn to handle real-world complaint scenarios using structured scripts and response templates, preparing them for the pressure of live patient interactions.
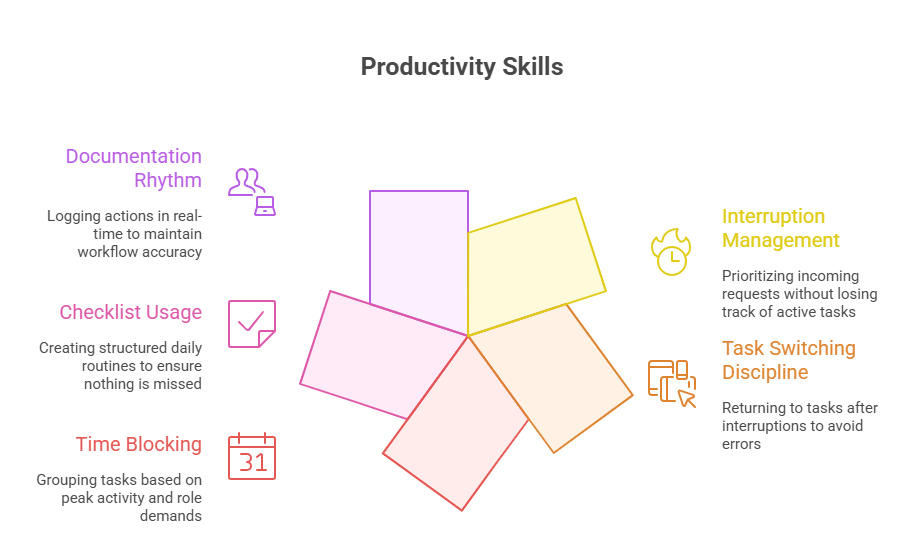
Time and Task Prioritization
Managing Interruptions in Busy Clinics
A typical clinic front desk handles over 50+ interruptions per shift — from walk-ins and calls to physician requests and system alerts. CMAAs who succeed don’t avoid chaos; they organize around it. Efficient task switching depends on structured interruption management rather than multitasking blindly.
Key techniques include:
Using color-coded flags or digital task boards to sort request urgency
Pre-setting voicemail redirects during peak patient intake times
Delegating non-clinical tasks during high-volume appointment windows
Logging each interruption to create a priority queue, not just mental lists
CMAAs must also train themselves to pause, confirm, and return to original tasks. Otherwise, documentation errors, misbooked appointments, and forgotten messages become systemic. Clinics that adopt this mindset reduce front-desk error rates by over 30%.
Creating a Daily Operational Checklist
Chaos dies where checklists live. The most reliable CMAAs operate off a dynamic, role-specific checklist they’ve refined through observation, feedback, and pattern recognition. This isn’t a generic task list — it’s a rhythm for the day.
A high-performing checklist includes:
Morning systems check (EHR access, fax queues, appointment confirmations)
Midday reset (referral follow-ups, claim rejections, lab call-backs)
End-of-day wrap-up (no-show flags, room closures, data backups)
Each task is tied to specific time blocks and roles. Checklists reduce mental fatigue, omission risk, and staff misalignment — making sure nothing falls through the cracks, even on the busiest Mondays. Our CMAA certification trains students to build and customize these workflows based on clinic size, specialty, and staffing model.
HIPAA and Data Handling Protocols
Do’s and Don’ts for Patient Privacy
HIPAA compliance isn’t just legal — it’s reputational armor. A single patient privacy breach can result in fines exceeding $50,000 per incident, plus irreversible trust loss. CMAAs must internalize the "minimum necessary standard" — only access, share, or discuss the data needed to complete a specific task.
Do:
Lock screens when stepping away, even momentarily
Verify caller identity before discussing any PHI
Use clinic-approved messaging systems, not personal texts or emails
Log all data access in the EHR audit trail
Don’t:
Discuss patient details in open spaces, including waiting rooms
Print, copy, or leave charts unattended at shared desks
Share login credentials or leave passwords visible
Skip HIPAA refresher trainings — they’re mandatory for certification renewal
With cybercrime targeting healthcare data, CMAAs are now first-line data guardians, not just support staff.
Safe Faxing, Emailing, and Record Transfers
Despite being outdated in other industries, faxing and emailing remain core workflows in medical offices. However, every transmission method carries exposure risk if protocols aren’t followed exactly.
To ensure secure record handling:
Always use cover sheets with disclaimers for faxes
Double-check recipient numbers and email addresses before sending
Use encrypted email systems or secure portals for sensitive data
Avoid sending full patient records unless explicitly authorized
Log the transmission in both the patient’s chart and the communication tracker
Record transfer protocols must also comply with state-specific retention rules, particularly for minors or chronic care patients. In our CMAA certification program, students practice handling real transfer requests across different systems, building habits that prevent critical mistakes in high-volume offices.
| Protocol Area | Best Practices | Why It Matters |
|---|---|---|
| Privacy Safeguards | Lock screens, restrict access, avoid open conversations about PHI | Prevents unauthorized exposure and ensures HIPAA compliance |
| Secure Communication | Use encrypted email/fax systems, verify recipient before sending | Protects sensitive data during digital or physical transfer |
| Data Sharing Controls | Follow “minimum necessary” rule; never overshare patient info | Limits risk of over-disclosure and audit penalties |
| Audit Trail Management | Log every access or change to patient records in EHR system | Creates accountability and legal traceability in case of breach |
| Ongoing Compliance Training | Participate in annual HIPAA training and refreshers | Keeps staff updated on rule changes and real-world violations |
Billing & Insurance Tasks
Verifying Coverage
Coverage verification is where billing accuracy begins. A CMAA who skips or mishandles this step can trigger claim rejections, delayed reimbursements, and frustrated patients. In today’s environment of high-deductible plans and frequent payer updates, verifying insurance details for every visit is no longer optional.
Key steps in verification:
Confirm policy number, group ID, plan type, and coverage limits
Check real-time eligibility through payer portals or clearinghouses
Document co-insurance, out-of-pocket max, and authorization needs
Verify if specialist visits require referrals or network restrictions
CMAAs must also record verification results inside the patient’s EHR and flag any potential denials for clinical or billing review. This step saves clinics an average of $4,300/month in avoidable losses.
Co-pay Collection Techniques
Collecting co-pays at the time of service ensures predictable cash flow and reduces billing friction. Yet many CMAAs hesitate to ask — or lack a script that makes the ask smooth and professional.
Effective co-pay collection includes:
Presenting the balance as a routine step (“Today’s co-pay is $25 — would you prefer card or cash?”)
Using visible signage that outlines co-pay policy
Ensuring private, respectful handling — not in the middle of a crowded lobby
Flagging non-payment and re-attempting at checkout
With collection at time-of-service exceeding 92% success when done correctly, training CMAAs in tone, confidence, and policy awareness is critical. Our CMAA certification includes patient payment simulations, so graduates can confidently handle both face-to-face and phone collections.
| Task | Execution Steps | Impact on Practice |
|---|---|---|
| Coverage Verification | Check eligibility, plan ID, copays, and pre-auth needs | Prevents denied claims and ensures clean billing submissions |
| Copay Collection | Politely request payment before visit; offer receipts and options | Improves revenue cycle and reduces collection risk |
| Claim Accuracy Support | Double-check patient info, ICD/CPT links, and visit type | Decreases rejections and administrative rework |
| Billing Communication | Flag complex cases for billing staff; use structured notes | Speeds up issue resolution and improves team coordination |
| Patient Billing Education | Explain copays, deductibles, and out-of-pocket differences | Reduces patient confusion and future disputes |
Learn These Office Skills in Our CMAA Certification
Scenario-Based Training
Most programs teach definitions — we teach decision-making under pressure. Our CMAA certification is built around real clinical workflows, not outdated textbooks. You’ll step into live scenarios where you must schedule urgent referrals, de-escalate upset patients, and spot errors in simulated EHRs — just like you would in a real clinic.
In these hands-on modules, you’ll:
Respond to scheduling challenges based on provider rules and payer logic
Practice patient intake scripts for various clinical specialties
Navigate conflicting priorities during peak hours without compromising accuracy
Communicate with professionalism across calls, emails, and in-person moments
Every scenario ends with feedback from certified instructors who’ve worked in high-volume offices. You don’t just memorize procedures — you train like it’s day one on the job.
Real Case Files in Practice Labs
What sets our certification apart is access to anonymized patient case files from actual clinics. You’ll process insurance verifications, correct billing entries, and complete record transfers based on real 2024–2025 documentation.
Inside the lab, you’ll:
Audit intake forms for missing consent or insurance data
Perform full appointment-to-claim lifecycle tracking
Flag privacy violations and submit formal documentation reports
Work within cloud-based systems that replicate what’s used in top outpatient centers
This isn’t just training. It’s skillproofing for real-world medical office management. By the time you finish, you'll be prepared for fast-paced clinical environments — and you’ll have the confidence to handle front-desk chaos, compliance risks, and high-stakes patient interactions with zero hesitation.
Frequently Asked Questions
-
A CMAA manages the non-clinical side of patient care, ensuring that every administrative task supports medical accuracy and efficiency. This includes checking in patients, verifying insurance, scheduling appointments, maintaining HIPAA-compliant records, and coordinating with physicians, billing departments, and pharmacies. In many clinics, CMAAs are the first and last point of contact for patients — meaning they shape both the experience and the outcome. They also act as the gatekeepers for compliance, flagging potential errors in documentation or coverage before they escalate. With the rise of telehealth and automated billing, CMAAs also need to be tech-savvy and capable of working across EHR systems, insurance portals, and patient engagement platforms in real time.
-
While a receptionist answers calls and greets patients, a CMAA has clinical-administrative authority. Unlike general medical assistants who focus on taking vitals or assisting doctors, CMAAs specialize in managing the entire patient flow on the administrative side. They’re trained to understand insurance, compliance, coding, and scheduling logic — not just basic clerical tasks. Most importantly, CMAAs are certified to handle protected health information (PHI) with full HIPAA compliance training. They're also expected to operate EHR platforms, coordinate follow-ups, and resolve billing disputes — tasks that a general receptionist typically isn’t trained for. In essence, a CMAA blends front-desk precision with backend accountability, making them essential to a clinic’s financial and operational health.
-
While not always legally required, CMAA certification is increasingly expected by employers — especially in competitive or high-volume environments. Clinics and hospitals prefer certified candidates because it ensures that the person has standardized training in HIPAA, EHR, scheduling, and insurance verification. Certification also reduces onboarding time and lowers the risk of compliance errors, which can lead to fines or revenue loss. In some states and organizations, CMAA credentials are a prerequisite for advancement to roles like office manager, billing coordinator, or lead scheduler. Many employers now list “CMAA preferred or required” in their job listings to ensure baseline skills. Certification also increases salary potential and job security in saturated markets.
-
Top-performing CMAAs must be fluent in insurance verification, accurate data entry, time-blocked scheduling, and EHR navigation. In 2025, these skills now include managing digital patient portals, coordinating remote visits, and handling sensitive record transfers with encrypted systems. Soft skills are just as vital — particularly the ability to de-escalate frustrated patients and communicate with empathy under pressure. Task prioritization is also essential: a CMAA must know how to triage calls, handle walk-ins, and support clinicians all at once. The ability to maintain calm while resolving multiple admin tasks simultaneously is what separates entry-level staff from high-impact professionals. This is why strong scenario-based training is critical in any certification program.
-
CMAAs are trained to follow the minimum necessary standard — accessing and sharing only what’s needed to complete a task. This includes securing digital and printed records, locking screens when away, verifying identities before sharing information, and using encrypted platforms for record transmission. In many practices, CMAAs are also responsible for flagging privacy violations and conducting internal chart audits for compliance. They must avoid casual discussions about patient information in public areas and are prohibited from sharing logins or passwords. Certification programs like ours teach specific workflows for secure faxing, emailing, and document storage, giving CMAAs the tools to actively safeguard patient privacy every day.
-
Modern CMAAs must master Electronic Health Records (EHR) systems, insurance clearinghouses, appointment scheduling software, and secure messaging platforms. They also need to use practice management systems for billing, prior authorization, and inventory control. Familiarity with platforms like Epic, Cerner, Athenahealth, and Kareo gives CMAAs an edge in job placement. In multi-provider clinics, they must know how to navigate multiple calendars, flag insurance issues, and process real-time eligibility checks. As healthcare becomes more digitized, CMAAs also interact with patient portals, mobile intake forms, and cloud-based communication systems. Certification programs that provide hands-on simulations with these tools better prepare students for fast-paced, tech-driven offices.
-
Absolutely. Many CMAAs move into roles like office manager, revenue cycle analyst, or compliance coordinator within 1–3 years, especially in larger practices or health systems. Employers value CMAAs who demonstrate leadership over workflows, vendor coordination, or patient escalation handling. With added experience or cross-training in billing and coding, CMAAs can transition into medical billing specialist or claims resolution lead roles. Those who enjoy the training side may become clinical admin educators or take on EHR superuser positions. The certification gives you a career foundation — but the daily experience, continuous learning, and accountability mindset are what unlock upward mobility in this field.
Final Thoughts
Efficient medical office management isn’t about multitasking — it’s about mastering repeatable systems, precision communication, and regulatory discipline. The Certified Medical Administrative Assistant plays a critical role in making sure clinics run smoothly, patients are cared for respectfully, and nothing falls through the cracks operationally.
Whether it’s verifying coverage, calming an upset patient, or correcting EHR entries, CMAAs carry the frontline responsibility for both revenue and reputation. These aren’t soft skills — they’re essential medical business functions. And they require training that mirrors the pressure, pace, and complexity of real healthcare settings.
If you’re ready to lead from the front desk — with confidence, accuracy, and compliance — our CMAA certification program gives you every skill, system, and scenario you need to succeed in today’s fast-paced medical world.
Poll: Which administrative skill do you believe is most essential for CMAAs in 2025?